100 Years, 100 Stories
Hannah Wise
Virginia Mason Seattle
“I started working for Virginia Mason in the Ophthalmology department in March 2017. In less than six weeks, I became a patient myself and saw all the ins and outs of the hospital. For six months prior to that, I had a persistent cough that started when I was eight months pregnant with my daughter. I was told then that I had acid reflux, which was causing my cough. My symptoms improved after my daughter was born, but by April the cough returned with a vengeance. In late April 2017, my cough had become so bad that I was coughing up blood. By 4 pm, I thought I should see someone before I went home. I took the elevator up to General Internal Medicine and asked if any provider could see me. A triage nurse brought me into a room and I showed her the pictures of the blood I had expelled. She sent me straight to the Emergency Department and did not let me talk her out of it. I walked myself to Jones Level 7 and they immediately got me in for a CT scan. I was diagnosed with a carcinoid tumor that was completely occluding my left lung. I was an otherwise healthy 26-year-old so this came completely out of left field. I was admitted and the next day I met Dr. Hubka, who later removed the tumor and did my partial lobectomy a few months later. I was already impressed by Virginia Mason’s reputation, which is what attracted me to the job. But after becoming a patient myself, I am so proud to be a part of this amazing organization that is saving lives, mine included.”

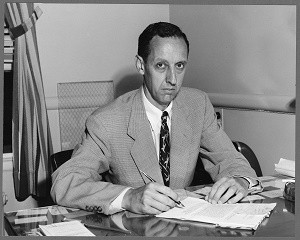
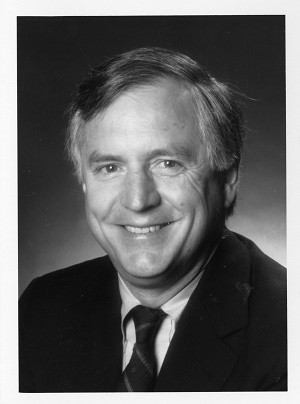
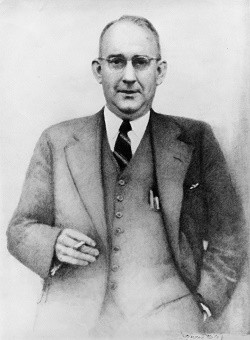
Virginia Mason Co-founder James Tate Mason Sr., MD
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
Dr. Mason was born May 20, 1882 in Lahore, Va., the son of a physician who had served the Confederacy under Stonewall Jackson. His mother was the daughter of a prominent Virginia colonial family. At 14, he entered the Locust-vale Military Academy, where he distinguished himself more on the baseball field than in the classroom. In 1901, he entered the University of Virginia Medical School and graduated in 1905 as one of the most popular students in his class. After medical school, he spent two years at the Philadelphia Polyclinic (the post-graduate school of the University of Pennsylvania) followed by serving as a resident at the Municipal Hospital of Philadelphia for the treatment of contagious diseases. In 1907, with his internships completed, he signed on as a ship’s surgeon aboard a steamship bound for Seattle by way of Cape Horn. The position offered $100 and a return railroad ticket home. However, he never used the ticket home. Arriving in Seattle in mid-summer with $50, he liked what he saw of the Pacific Northwest and, within two weeks, was hired as company surgeon – at the age of 25 – for a coal company in Black Diamond, Wash. In 1909, he returned to Seattle to practice there. Within a few months, he welcomed the opportunity to become physician to the county jail. He was married in 1911 and in 1913 he and his wife, Laura, welcomed the first of their three children. In the next few years, Dr. Mason earned the respect of his patients as well as the city’s business and political leaders. He was elected coroner of King County and organized an Anatomical Club with his colleagues, which later merged with the Seattle Surgical Society. From 1917 to 1920, he was superintendent and surgeon of the King County Hospital. And in 1917, he organized a partnership with five doctors and two associates to form the Mason-Blackford-Dwyer Clinic, which would eventually become Virginia Mason Medical Center.
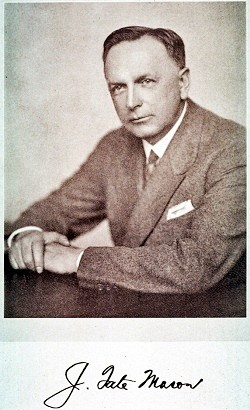
James Tate Mason Sr., MD
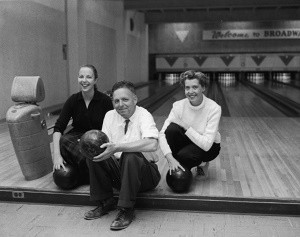
Seattle TV Icon, J. P. Patches, Visited Virginia Mason in 1970
Julius Pierpont “J. P.” Patches was a clown and the main character on The J. P. Patches Show, an Emmy Award-winning local children’s television show on Seattle station KIRO TV, which was produced from 1958 to 1981. J. P. Patches was played by show creator and Seattle children’s entertainer, Chris Wedes (1928-2012). When the show ended in 1981, The J. P. Patches Show was one of the longest-running, locally produced children’s TV programs in the United States.
In 1970, J. P. Patches visited Virginia Mason as part of the team member recognition program, PRIDE (Professional Results In Daily Effort). That year, Patches emceed the staff “Hobby Show” competition. Patches also visited with young patients in the hospital to provide laughter and encouragement.
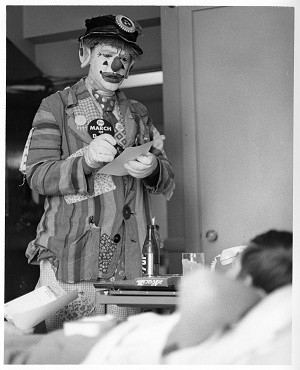
JP Patches brightens the day of a young patient at Virginia Mason in 1970.
Fred Savaglio
Virginia Mason Seattle
“I have a lot of stories about wonderful experiences at Virginia Mason. As an example, a very moving story was in the aftermath of the Hudson Arms fire when the six or seven evacuated residents were gazing up at the apartments they could not return to. Among them were three who owned cats which, at that time, may have been lost during the fire or fire department operations. Eventually, we were able to gain permission for Virginia Mason engineers to go in and look for the cats. About 45 minutes later, the three engineers came out and each was holding an agitated cat. The residents were emotionally drained and a lot of tears flowed. A second memorable story that night was when the residents were being processed by the Red Cross to shelters where they would remain until other more permanent housing could be found. Prior to the Red Cross transport, it became known that each resident had medications they would need that night. Nancy Hendler was on scene and she patiently took each resident’s medical history and with her Nurse Practitioner’s prescriptive authority wrote all the scripts they would need for the coming days. The Red Cross then went out got those prescriptions filled. So, many times Virginia Mason staff have stood strong in tough situations. I think of so many unsung heroes and heroines. Although their names have long left my memory, I was very moved each time team members came through. These are a couple of the fond memories about Virginia Mason that I wanted to share.”
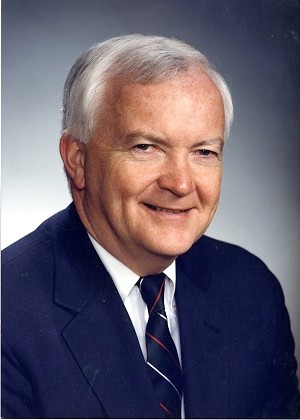
John Dare: Mason Clinic, Virginia Mason Hospital Administrator 1935-1977
(Excerpted from an interview by William Steenrod Jr., MD, on Oct. 11, 1985)
John Dare was an administrator in The Mason Clinic and Virginia Mason Hospital from 1935 to 1977. His father was Lewis Dare, the first administrator.
“I went to the University of Washington and graduated in business administration. Eddie Carlson* was a classmate. He was broke. We were all broke. There weren’t any jobs around. Eddie had to quit school and went to work for Western Hotels. Most of the guys graduating were going home to live with their parents because there weren’t any jobs in sight. Believe me, it was bleak.
One day, Eddie called and said, “I think there’s a job down here at the Roosevelt Hotel. Come down and get here quick. I got the job as a night auditor for Western Hotels at the Roosevelt Hotel. Eddie was a room clerk and we worked there for 18 months together. He then took off and went up to run the President Hotel in Mount Vernon, which was his first command in the hotel business.
About the same time in 1935, I got a call from Dr. Tate Mason who said, ‘I want to talk with you.’ It came as a great surprise. But having nothing else to do, I came up the hill and talked with Dr. Mason and my father. They had decided that due to the growth of the Mason Clinic and Virginia Mason Hospital, they wanted to put another guy into the organization with a business background.
A few days later, they called me and told me if I wanted to the leave the hotel business, I could come up here and learn this racket. I came up the day after Labor Day 1935.”
(* Leader in the hospitality industry, driving force behind the Century 21 World’s Fair, and CEO of United Airlines.)
Gigi Gempesaw, RN: Director, Acute Care Services
Gigi Gempesaw, RN, started work in a Virginia Mason pharmacy as a nursing student 34 years ago. She remembers delivering medications to hospital rooms and observing the patient-nurse relationship. The one-to-one interaction struck her as extraordinary.
“I decided then that I wanted to be that person making a connection with the patient,” said Gempesaw. “As nurses, we’re given the gift of being there at someone’s most vulnerable time.”
She remembers working in different organizations as a nursing student, but none felt as welcoming to her as Virginia Mason. Encouraged by a sense of inclusiveness and respect among team members and leaders alike, Gempesaw knew she would have the foundation to take good care of patients. Today, no matter who she calls on during the work day, she knows their commitment to the patient is equal to her own.
For Gempesaw, it all comes back to valuing relationships, with patients and team members. Couple that with a healthy resiliency, and you will have what it takes to thrive as a nurse.
“Whether you work somewhere for three days or 30 years, make those connections,” she said. “If you’re the nurse helping a patient at 2 a.m., it’s a moment they may always remember. I can’t imagine another profession that would bring the same joy to my life.”

Gigi Gempesaw, RN: Director, Acute Care Services
Anna J. Fraser, RN – First hospital and nursing service superintendent
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
Anna Fraser, RN, graduated from Saint Joseph’s School of Nursing in Tacoma. She worked for Dr. James Tate Mason in 1918 and joined him and his associates when Virginia Mason Hospital was founded in 1920. She held the position of superintendent of the hospital and nursing service until her retirement in 1944.
It was a proud Fraser who enrolled three students in the Virginia Mason Hospital School of Nursing in 1921 and made arrangements for their graduation on May 7, 1925. Each succeeding year, the graduating class increased in size.
Fraser was referred to as a superintendent of nurses who guided with tenacity of purpose and disciplined a modest (nursing) family of her own.
In 1929, students were first taught by professors from Seattle College and in 1936 the Student Body Association was organized. The first capping ceremony for students of the Virginia Mason Hospital School of Nursing was held in January 1938. In 1946, the ceremony moved to Blackford Hall and continued every year until the training program combined with the baccalaureate nursing program at the University of Washington School of Nursing in 1957.
Fraser was loved and admired by the students. After a 26-year career at Virginia Mason, she retired from the well-organized and fast developing nursing training school and growing, 150-bed hospital.
In appreciation for her countless contributions to the training program, the school library was named in her honor by the alumnae and students in May 1950.

Charleen Tachibana, Senior VP, CNO: When a Calling Becomes a Call to Action
Every day Charleen Tachibana, RN, works to keeps nurses at the bedsides of patients. It’s a basic idea that has required a career’s worth of passion and innovation. It called for implementing a care management system never tried in a health care setting. And it produced outstanding results in patient health and safety, efficient practices and personal care time for patients.
Since starting as a student nurse at Virginia Mason in 1976, Tachibana has embraced new learning opportunities at every turn, committing herself to the development of nurses in leadership. In recognition of her vision and accomplishments in advancing clinical care, Charleen was honored as a Fellow by the American Academy of Nursing in 2012.
“Charleen’s experiences as a nurse at the bedside give her an invaluable perspective as a transformative leader,” said Sarah Patterson, executive director, Virginia Mason Institute. “Charleen is one of those rare leaders who is at ease talking and thinking in terms of the systems of care, but is also able to understand and articulate the impact of a decision on the individual patient.”
Guide. Mentor. Visionary. The consummate caring professional. Inspirational. A force for change. These are some of the words Charleen’s colleagues use to describe her. Tachibana has said the best part about nursing is making a difference in peoples’ lives. But she also finds great fulfillment in the teamwork and sense of shared purpose at Virginia Mason.
“Having worked with Charleen since the day I arrived at Virginia Mason in 1978, I have been able to watch her develop from a superb cardiac and critical care nurse to an exceptional leader and administrator,” said Gary S. Kaplan, MD, chairman and CEO, Virginia Mason Health System. “She combines the very best of nursing practice with the vision, caring and passion to truly transform health care.”

Team Member-Supported Charity Auctions in the ’80s and ’90s
(Excerpted from the book, “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”)
“The medical center’s team member Sweet Charity Auction was started in 1984 to raise additional funds to help care for patients in need. In 10 years, team members raised more than $350,000. Janet Walthew from the business office provided the spark and leadership and identified a group of very committed team members to make it work.
“At one auction, the fire department arrived when Bob Weissman, MD, was demonstrating a chainsaw and accidently set off the hospital’s fire alarm system. (The item he was auctioning was a vasectomy.) On another occasion, Bill Traverso, MD, brought his llamas for a petting zoo at the entrance of the hospital, which was a traffic stopper. And at a different auction, part of Terry Avenue was closed for a daytime “Western Street Dance,” which was also a great morale booster.”
One of the First Hospitals in the U.S. to Allow Fathers in Delivery Rooms
(Excerpted from ‘Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995’)
“In the 1940s and 1950s, innovations in medicine were rapidly occurring throughout the country. One controversial innovation was the move to permit fathers to enter delivery rooms and participate in the birthing process. This was a decision that was widely criticized by some who thought it would be risky for the father – who might interrupt things by fainting – and delivering mother.
‘After all,’ opponents said, ‘we are there to take care of the mother and child, not worry about the husband.’
“In the late 1940s, Virginia Mason became one of first hospitals in the nation to allow fathers in the delivery room. Leadership for the change came from Robert Rutherford, MD, a member of the visiting staff.
“In 1955, LIFE magazine published a related story, which included a photo of a father in a delivery room at Virginia Mason.”
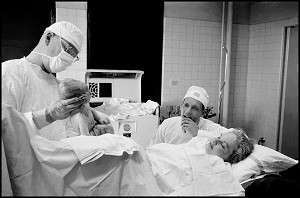
©Burt Glinn / Magnum Photos One of the First Hospitals in the U.S. to Allow Fathers in Delivery Rooms
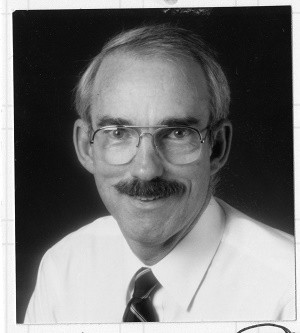
Jim Benson, MD: Practiced at Virginia Mason Starting in 1975
(Excerpted from an interview by John Kirkpatrick, MD, on Sept. 24, 2015)
“Soon after Dr. Paul Fredlund arrived here, he recruited me, which was pretty nice given the fact that there was no position. The Department of Endocrinology and Medicine was kind enough to create a position that didn’t exist. So, we were loaded with endocrinologists at that point, which was a lot of fun. One of the advantages of being collaborative and collegial in the department was that your experience expanded exponentially. At the end of a week when I hadn’t seen many interesting cases or pathology personally, I would realize that I’d seen a bunch of great cases. Because someone would grab me out of a room and say, ‘What do you think we ought to do about this complicated case?’
“The highlight of my career at Virginia Mason was when we did a bunch of research on the insulin pump about 1985. Drs. Bill Camberlane and Bob Sherwin at Yale thought there should be a better way to deliver insulin than by injection twice a day. They literally dusted off a chemotherapy unit or infusion system and said, ‘We ought to toy with this thing and see if it’ll work.’ It was called the blue brick. You had to change the basal rates with a screwdriver. They did their first six and reported a dramatic improvement.
“So, we thought this is something we should get interested in. We toyed with the idea of flying back to Yale, but they were out here for a meeting. Dr. Sherwin said, ‘There’s really nothing to it. I can call you or write you with the protocol on how to dilute the insulin and how we calculate the basal rates. You guys can do it.’ We each got one blue brick from the manufacturer and one patient each and tried it out. We were impressed and adopted it whole-hog.
“One of the highlights of my academic career was about a year later. We were invited back to Minnesota to a company meeting to present everybody’s experiences and suggestions for new pumps. I was nominated by the department to represent us. I showed up late, got up the next morning and realized that people there were all the big names in diabetes. These were heads of departments, people I’d been reading about for years and there was me.
“I got up and said, ‘I’m from Virginia Mason Clinic and am here to report on our first 100 cases.’ There was a visible gulp from the crowd because we had taken it on full-speed. That led to two articles in the New England Journal authored by Dr. Bob Mecklenburg, which featured all of us. I thought that was pretty inspiring!
“Another unique aspect about Virginia Mason back in those days was that surgical residents rotated on the medicine service and medical residents rotated on the surgical service. Everybody knew everybody and we all got along well. Before there was a pyramid with the patient at the top, we already knew that. Competition between surgeons and medical people didn’t make sense. What made sense was taking care of patients. I think that interaction among different services was highly valuable.”
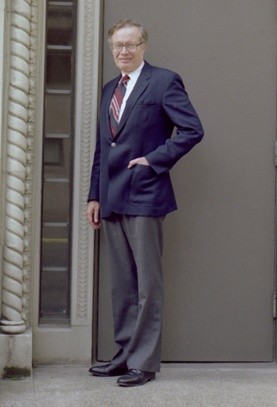
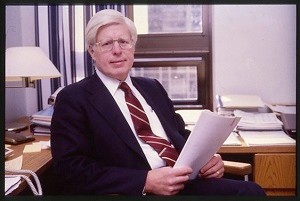
Austin Ross (1929-2020): Longtime Influential Leader at Virginia Mason
Austin Ross joined Virginia Mason Hospital in 1955 as the organization’s first administrative resident and retired in 1991 as executive administrator. Over his 36-year tenure, he was instrumental in helping shape Virginia Mason into what it is today, while becoming a nationally acclaimed expert and leader in the health care industry.
In July 1968, he wrote this article, headlined “Looking Ahead,” for the staff newsletter:
“The completion of the West Wing – East Wing development was obviously a significant milestone in the continuing program of modernizing and updating our medical center facilities. Although the dust has settled, and we can turn once again to a more normal course of daily events, we must focus our attention during the several months ahead on several important and, somewhat neglected, programs.
The first of these relates to brushing up on the ‘gracefulness of care’ rendered our patients. The patient who enters our institution looks for more than just sophistication in their care. They expect to be treated as an individual by people who have warmth and understanding and who will do more than the minimum to make them comfortable. It is our firm belief that the employee who has these qualities of warmth and understanding makes a considerable contribution to that patient’s recuperative powers. The attitude of the patient in their surroundings has a bearing on their acceptance of medical advice and treatment.
Virginia Mason Hospital has always had a tradition of caring. During construction and growing periods, some of these fine edges of personal service and personal consideration may become rough. It is our sincere hope that jointly, over the next several months, we can concentrate as a group on rededicating ourselves to improving on some of these finer practices.
What do we mean when we talk of the ‘gracefulness of care?’ Some specific examples:
You become aware, by listening, of the extremely high noise levels in patient care areas – the squeaky casters on the equipment, loud voices, the too frequent use of the page system for individual staff convenience. You watch for the softer touches, for example, how are patients transported through the hospital – with cold dispatch or with friendliness and consideration? Gracefulness has to do with the types of conversations that take place in elevators with patients present and the many other indicators of sensitivity.
The list of do’s and don’ts could be endless, but the point to emphasize is that each of our patients need to be treated as we would expect ourselves treated in a similar situation, and with respect to privacy and medical condition. If problems occur – and they are bound to periodically – then, since the patient is a guest in our home, we should right those wrongs by apology or by special attention.
We would urge your whole-hearted participation in the months ahead to bring additional warmth and caring into our patients’ lives. This is our tradition and, although we may be doing ‘all right,’ I think we can all admit that we could do better.”
John Ryan, MD: Practiced at Virginia Mason Starting in 1978
(Excerpted from an interview by David Wilma on May 30, 2018)
“My father was a surgeon, a urologist. He was associated with Tate Mason, the son of the founder of Virginia Mason, so I was aware of the organization. When I started my surgical residency at Massachusetts General Hospital in Boston, Virginia Mason was well known there.
In 1977, I wrote a letter saying I was a young guy looking for a job. There were many jobs open in surgery at the time and I interviewed all over, including at the University of Washington and Harborview. Harborview was a trauma hospital and wasn’t really interested in trauma at all. So, I left Harborview and walked down to Virginia Mason. I came in the door and for some reason thought, this is the place. I was impressed that nobody was talking about leaving. Everyone seemed to stay there their whole career and that meant something to me.
The thing that really made it good for me is that I knew it had a good local and national reputation, which was enhanced by the way surgical staff related to residents, called house staff. Each surgeon had two residents dedicated to them around the clock.”
Elizabeth Braun
Virginia Mason
“I have had the delight and honor of both working for Virginia Mason and being a patient since 1988. I have watched the organization add or replace numerous clinics and hospital additions. The buildings are my children. Designing, building and watching them evolve has been tremendously satisfying. The care is what excites me about coming to work every day! I have watched as my family’s lives, and my own life, were literally saved several times because of our outstanding care. I know this comes from our commitment to being the quality leader, and the creativity and devotion of the staff. Thank you all!”
Laura Jeffs
Virginia Mason Seattle
“Founded in 1984 by Virginia Mason’s first psychiatrist, Ted Rynearson, MD, and Jacki Meurk, former board member, the Separation and Loss (Grief Services) department offers individual and group support to sudden, traumatic death (homicide, suicide, accident, overdose and illness) survivors using Dr. Ted Rynearson’s Restorative Retelling model. Dr. Rynearson literally “knocked on doors” at the Department of Justice in Washington, DC, to share about the services to be offered and request grant funding to support the program. Partially funded since 1998 through a DOJ crime victim service grant, the team has expanded services to include: critical incident debriefs within Virginia Mason and in the community; Restorative Retelling Facilitator trainings; regional and national trainings on traumatic death and related topics; and consultation. Several group intervention outcome studies have been published, and Dr. Rynearson won the Association of Death Education and Counseling (ADEC) researcher of the year award in 2013. He has consulted with Israeli and Palestinian clinicians on the model, as well as with the Federal Bureau of Investigation. The small team of Laura Takacs, Laura Jeffs and Dr. Ted Rynearson is grateful to Virginia Mason for its ongoing support.”

(left to right) Edward Rynearson, MD, Laura Takacs, LICSW, MPH, and Laura Jeffs
Lauren Lindeman: Facing Cancer with the Team Behind You
(This article was written for Virginia Mason’s Health & Wellness blog in 2015.)
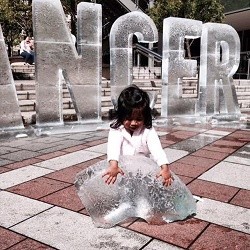
One sunny day in downtown Seattle, Virginia Mason made cancer disappear. Five-foot tall letters made of ice spelled the disease, then slowly broke apart into icy rubble under blue sky at Westlake Park. Part of the ‘See What’s Happening to Cancer’ campaign, Virginia Mason physicians and health care experts were near the sculpture to provide information on cancer prevention and screening.
We asked Virginia Mason team member and breast cancer survivor Lauren Lindeman to talk about how she experienced the event.
How was this event personal to you?
“In January 2015, I was diagnosed with very early stage breast cancer. The early detection made possible by 3D mammography meant I could undergo a lumpectomy, have radiation just once during the surgery, and not need chemotherapy at all. Even though we’ve all heard the words ‘early detection’ like a mantra, it’s finally real for me. It may take some time and persistence, but cancer can be defeated. I loved how the ice sculpture symbolized that in such a tangible and visual way.”
What did it mean to you as a Virginia Mason team member?
“Many members of our leadership team made a special trip down to see and support this amazing concept that cancer can and will be overcome. Throughout the day, team members from all areas and job descriptions used their breaks to come see the sculpture. It gave me a true sense of pride in our Virginia Mason family and reflected the commitment we all feel in our role as patient ambassadors.”
How did it feel to be at the sculpture site?
“Joy and excitement within myself and also from the crowd. Who knew it could be so exciting to watch the letter E disintegrate or see a chunk of a C crash loudly to the ground, or better yet, watch a survivor pose for a picture where she was ‘kicking cancer?’”
What did you see and hear from others?
“Throughout the day, people shared incredible stories of their own battles with cancer. Either they had been touched by cancer personally or experienced it with loved ones. Those who had lost loved ones to cancer were especially supportive of our efforts. Everyone wants to rally together in this fight, and that was truly amazing to see.”
Any particular moments that stood out for you?
“After hearing my story, several women admitted that they were way overdue for a mammogram and committed to get in right away. There was a beautiful little girl who was trying to melt a fallen chunk of the letter C with her tiny hands. An 80-year-old man shared his story of beating prostate cancer and being able to visit his children in Seattle. Then there was the roar of the crowd every time another letter bit the dust.”
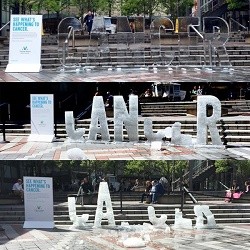

Lauren Lindeman
Birth of Nuclear Medicine
(Excerpted from “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”)
“Soon after World War II ended, the X-ray Department experienced numerous changes. One, which had national importance, was development of the radioisotope. With the announcement of the atomic bomb, it became clear that radioisotopes might soon be available for clinical use. Thomas Carlile, MD, was especially intrigued with the potential clinical use of isotopes and spent the summer of 1947 studying medical applications of nuclear physics at the University of California. Soon after, he introduced radioactive phosphorus and iodine to the hospital early in 1948.
‘At the time, we had to do our own calibration,’ Dr. Carlile later said. ‘We didn’t receive commercially packaged isotopes as we do today. Rather, we received bulk materials from the Department of Energy’s National Laboratory in Oak Ridge, Tennessee. It arrived in huge, lead-shielded containers. We would have to take these raw isotopes and refine them for clinical use. At the time, we were supplying the University of Washington and Swedish Hospital’s Tumor Institute on the basis of the calibrations that we did here. I would work night after night with one of our residents calibrating these isotopes and getting them ready for human use.’
Ultimately, the need for standardization of radioactive isotopes on a national scale led to the formation of the Society of Nuclear Medicine, which was born in the Pacific Northwest and then developed chapters across the country. Dr. Carlile was a founder and became the society’s first president in 1953.”
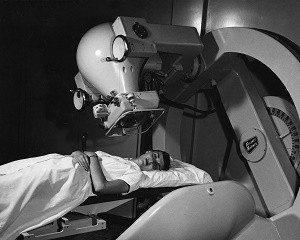
1957: First Cobalt-60 cancer treatment in the Pacific Northwest was offered at Virginia Mason.
First Radiologist at Virginia Mason
(Excerpted from an interview with Thomas Carlile, MD, by William Steenrod Jr., MD, on April 16, 1988)
“There was a time when Virginia Mason was known as the Mason-Blackford-Dwyer Clinic. Dr. Maurice Dwyer was Dr. Mason’s first partner. In 1914, when Dr. Mason came to Seattle, Dr. Dwyer was in general practice.
Dr. Dwyer was a short, frail man who had a bad limp from hip dysplasia. Compared to Dr. Mason, Dr. Dwyer wasn’t a particularly dominant figure, but complemented him well as his right-hand man. When Dr. Blackford came out from Rochester, Minnesota, it became the Mason-Blackford-Dwyer Clinic. When the Dowlings came along, it was decided they couldn’t keep adding the names of every doctor added to the group. I think Dr. Palmer was the last one to be added. It was about that time that they finally dropped everybody’s name, except Dr. Mason.
Dr. Dwyer became interested in X-ray early on and followed its development in the Northwest. He began attending X-ray meetings and spent some time at Mayo and other reputable clinics in Washington, DC. When The Mason Clinic formed its Board of Internal Medicine, Dr. Dwyer was honored as a grandfather of the specialty. By the early 1920s, he was a leading radiologist in Seattle – one of the first two or three.
Dr. Dwyer branched out into X-ray therapy and installed the first X-ray therapy unit at The Mason Clinic. In 1935, he was granted a grandfather certificate in radiology. He held certificates in internal medicine and radiology. Since the internal medicine doctors told him he had to choose between them, Dr. Dwyer kept his radiology certificate.
Unfortunately, he had hypertension and his vision was failing. When Dr. Dwyer died in 1944, we definitely missed him.
The Seattle radiologists were particularly good to me after Dr. Dwyer’s death. They were very generous with their time. Harold Nichols, MD, who was a very prominent radiologist, offered me a job, but I wanted to stay at The Mason Clinic. So, I took my boards in 1945 and, soon after, became a partner. I ran the Department of Radiology by myself for two years for a salary of $500 per month.”

Maurice Dwyer, MD (left) with J. Tate Mason, MD
Virginia Mason Co-founder John Minor Blackford, MD
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
In 1917, Dr. Blackford was practicing medicine at the Mayo Clinic in Rochester, Minn. when Dr. Mason – who was attending a medical conference at Mayo – met him. The two became fast friends and Dr. Mason then asked Dr. Blackford to join him in practice in Seattle. Dr. Blackford had been active in research in cardiology and diseases of the thyroid gland at the Mayo Clinic and later, high blood pressure and gastroenterology. He participated in the installation at Virginia Mason of the first electrocardiograph machine west of the Mississippi River. He performed clinical research while in practice and presented a number of original articles to medial organizations, especially in the field of gastroenterology. He also encouraged members of the medical staff, especially younger physicians, to become involved in clinical research and present papers whenever possible. Dr. Blackford was a large and friendly man who enjoyed a host of friends, both inside and outside the medical profession. He inspired a confidence in others and developed a large practice involving many community leaders. He enjoyed the respect of his medical colleagues and was often called in consultation for medical problems. He was a genius at analyzing the problems of patients and always added something to the diagnosis. Dr. Blackford was a husband, father of three as well as an ardent bridge player and yachtsman. He was very proud of his yacht that bore the name of his youngest daughter, Sally Bruce. He was an inveterate smoker of cigarettes and always kept a tin of fifty cigarettes in his pocket. He had a particular type of cigarette cough which, at times, was severe enough to render him temporarily to lose consciousness. His peers felt that his cigarette smoking probably contributed to his death from pneumonia.
John M. Blackford, MD
Eileen Dunning
Virginia Mason Seattle
“As a proud Virginia Mason retiree, I’ve recommended the health system to a number of people, including three family members, friends and several people from my church. Sometimes it’s been a matter of helping them find a provider who I view as exceptional and other times it’s been something that required more immediate attention. Regardless, Virginia Mason has never disappointed.
A person very close to me had a myocardial infarction and was deciding between having it stented versus bypass surgery. Although she had been a longtime patient of another Seattle-based health system, I persuaded her to obtain a second opinion from Virginia Mason interventional cardiologist Wayne Hwang, MD. Dr. Hwang discovered a blocked carotid artery, which had gone overlooked where my friend had previously been seen. She decided to have carotid artery and coronary artery bypass surgeries at Virginia Mason. My friend, her family and I were so pleased with the medical and nursing care she received. A few years later, my friend developed unrelated, acute complications and died in the Critical Care Unit at Virginia Mason. Her care could not have been better and was provided with incredible compassion and respect for her family.
I am always incredibly proud to recommend Virginia Mason to people I care about. I respect the expertise that I know the health system seeks and maintains among their providers. I also respect the expertise of the nurses and other professionals caring for patients.”
Sandy Novak: Virginia Mason Administrator Starting in 1978
(Excerpted from an interview with David Wilma on Jan. 7, 2019)
“When I was working in human resources (HR) The Westin Seattle, I heard that the director of HR at The Mason Clinic had accepted a job at Boeing. A colleague thought it would be a good opportunity. So, I contacted Austin Ross and met Bob Boyle, senior assistant administrator, at Trader Vic’s restaurant because I wanted to impress him. In June 1978, Austin hired me as HR director for everyone but physicians. That was out of the chairman’s office.
“After a few years in HR, I decided I wanted to be in a broader operation role. When I arrived at Virginia Mason, there were no female physicians. Even me being in an administrative role was pretty innovative at the time. So, I was always aware that I had to be better than the best. I was very driven to make sure I was making a positive impression. I felt like I had a lot of responsibility being one of the few women there. A few years later, Dr. Detweiler was hired as a pathologist with no thought that she would be a partner.
“Later on, a new assistant administrator position opened at the clinic. However, an administrative fellow was being groomed for the position. Despite feeling like I didn’t have much of a chance, I spoke with Austin Ross and told him I’d like to throw my hat in the ring. Being the reasonable administrator that he was, Austin said OK. Thankfully, unbeknownst to me, I had strong support from a number of physician leaders. The compromise was that we would have two positions and I would have one. After a year, the fellow would find something else.
“I really liked working for Austin. One of the smartest decisions he ever made was assigning one administrator to support each section. Every section head knew who their go-to person was. In some ways, this was more work for administration. But it helped develop closer ties between physicians and leadership. There was more of a collegial feeling than I saw in other organizations.
“Austin Ross was a masterful strategist who thought about the physician colleagues and how administrators should interact with them. That’s what his style was.”

Sandy Novak with Austin Ross
Roger C. Lindeman, MD: Practiced at Virginia Mason Starting in 1968
(Excerpted from a 2005 monograph by Dr. Lindeman and an interview in 1998)
“It was 1967, during my first year at Valley Forge General Hospital in Pennsylvania as a captain in the Army, that I had the pleasure of meeting Dr. Phil Jolly. He was applying for a position in the Department of Surgery at The Mason Clinic in Seattle. The Chief of Surgery from The Mason Clinic was coming to Valley Forge to watch him operate. I remember being impressed that The Mason Clinic was that careful in deciding whom to hire. Dr. Joel Baker observed closely as Dr. Jolly did two rather complicated cases. Needless to say, Dr. Jolly passed with flying colors and his future with The Mason Clinic was assured.
I had the opportunity to meet Dr. Baker and learn more about The Mason Clinic. He mentioned they were looking for a specialist in otology and neurotology, as their current otologist was about to retire. Shortly thereafter, I received an invitation from Dr. Baker, asking my wife, Lillian, and I to come to Seattle for a two- or three-day visit.
This was an impressive visit. I was presented with a full schedule of half-hour appointments with physicians in almost all specialties. There were visits and tours arranged for Lillian, as well. The final appointment for me was with Dr. John Walker, chairman of the clinic. I was surprised that he already knew so much about me. I will always remember Dr. Walker’s comments as he was describing the uniqueness of The Mason Clinic.
‘Here,’ he said, ‘our physicians have the opportunity to practice very high-quality health care in a setting of medical education and research. Most of us are very active in both clinical and academic endeavors. I think you would find in each section, and in each specialty, one or more physicians who know as much about their specialty as anyone in the country!’
Lillian liked Seattle and especially the people she had met. I couldn’t help but think what a privilege it would be to be able to teach, participate in clinical research and practice with outstanding physicians of like mind and common purpose. Before leaving, I met with Dr. Walker again. He made an offer and I accepted.
In March 1968, I was discharged from the Army and drove cross country to Seattle to join The Mason Clinic’s Otolaryngology section. Lillian and our three kids joined me soon after. My clinical practice grew rapidly and I enjoyed teaching otolaryngology residents at the University of Washington. Soon, we established an official rotation for UW residents at Virginia Mason Hospital.
Through the generosity of Mr. William G. Reed, we established the Reed Laboratory for Research in Otolaryngology. Our most significant contribution was probably a new surgical procedure called the tracheal diversion procedure. This is a reversible procedure designed to protect the lungs from aspiration pneumonia in patients who, at least temporarily, were experiencing laryngeal paralysis as a result of a brain tumor, stroke or other neurological disorder. I wrote the article describing this procedure, which soon became known as the Lindeman Procedure.
My practice continued to grow, mainly in otology and neurotology. We became a referral source for patients with acoustic tumors.
I could not have accomplished this work without the complete cooperation of Dr. John Tytus, section head of Neurosurgery at The Mason Clinic. Acoustic tumor surgery had long been considered within the domain of neurosurgeons. Many resisted this ‘invasion’ by neurotologists and refused to cooperate. This was partially true in Seattle, but not at The Mason Clinic. What an advantage it was to work as a team in a group practice setting. Neurosurgeons, locally and nationwide, eventually agreed to cooperate. But by that time, we had established a solid reputation and attracted patients from around the Pacific Northwest.
I think I was the 55th partner, so I would have been The Mason Clinic’s 55th doctor. We practiced just specialty care. We didn’t practice primary care until 1975. We were all located on one campus near downtown Seattle. We didn’t have any satellite clinics at the time. There was a wonderful esprit de corps, a wonderful collegiality that was present. The older doctors would say, ‘Well, it just isn’t like it used to be when we had nine partners and could have partners’ meetings in someone’s home.’
The people make it a great place to work. We have always tried to attract the very best physicians, nurses and administrators.
In February 1980, I was elected by the physician partners to be chairman of The Mason Clinic for a four-year term. There was a lot to learn despite my previous experience and participation in management courses. At The Mason Clinic, the physician chairman works closely with the clinic’s executive administrator. It was my good fortune to team up with Austin Ross, who was serving in that capacity. Austin was not only a highly skilled administrator, but a professor of health care administration at the University of Washington. What more could a new chairman ask for? It was a pleasure to work with Austin until his retirement in 1991.
I was reelected by the partnership for four additional four-year terms and served as chairman of The Mason Clinic – and later chairman and CEO of the medical center – from 1980 until my retirement in 2000.”
John Knab
Virginia Mason Seattle
“I remember being in the operating room one evening as a third or fourth year Virginia Mason anesthesia resident in 1996 or 1997. As I looked at the anesthesia machine, it began to wobble and shake, and I thought maybe I was inhaling too much sevoflurane. Then, as things began to shake throughout the room, including my colleagues and the patient, I realized that we were in the middle of an earthquake. My first and only!”
First Baby Born at Virginia Mason Franciscan Health Birth Center
“I had the privilege of being the first woman to give birth in the new Virginia Mason Franciscan Health Birth Center. In April 2020, while COVID-19 was turning the world upside down, I suddenly and unexpectedly became a single mother to my two young children, with No. 3 on the way. In my grief, Virginia Mason team members were a rock of stability and staff from Franciscan Women’s Health at Virginia Mason offered me their unwavering support, grace and strength through one of the darkest periods in my life. On the morning of Aug. 11, 2020, I arrived at the Birth Center tired and very ‘over it.’ Although I knew in advance it was a possibility and that staff knew I was coming, I was still surprised to learn I was first! There was a giddy, nervous energy in the air. Everyone was excited! My nurses respected my boundaries through the labor, offering me the encouragement I needed, while allowing me the space to labor on my own. Despite a valiant effort from the Anesthesia team to get me an epidural once the time came, the baby and my body had other plans. I transitioned quickly and, as the team brainstormed how to manage my unrelenting pain, I realized I would soon meet my newest child. A sea of familiar faces surrounded my bed, and at 5:45 p.m., my obstetrician safely delivered him and I lifted my son to my chest. Zachary entered this world surrounded by love. When I checked my phone several hours later, a slew of text messages from my peers revealed that the whole hospital knew he had arrived – a little light in a time of seemingly unrelenting darkness. I will forever be grateful for all the nurses and doctors who held my hand – literally and figuratively – through my pregnancy, birth and postpartum care. It was a huge relief to confidently place my trust, and my child’s health, in the hands of a competent and compassionate team. Thank you!” – Natalie Dively, NA-C, Critical Care, Virginia Mason Medical Center

Harold Dill
Virginia Mason Seattle
“My first introduction to Virginia Mason was in early 1959. I had just come out of military service and was hired by Northern Commercial Co., which had numerous stores in remote locations of Alaska. Each of their managers being sent north had to pass a physical examination administered by Virginia Mason. In subsequent years, it became an annual event as we all returned to Seattle for our managers meetings. My physician was Dr. Randolph Pillow. I will never forget him. I was so impressed with his patient skills and medical knowledge. He was my hero for many, many years.”

James Tate Mason Jr., MD: Virginia Mason Physician, Son of Founder
(Excerpted from a video interview in 1988)
“My professional life with my father was very limited. He died when I was 22 and in my first year of medical school. When I was a boy, I made many visits to the hospital. When I was six or seven, I went while the hospital was being built. My mom and dad were looking at what was going on. They looked up aghast at me four stories up in the scaffolding. That resulted in my first spanking.
“I remember my dad operating and teaching all the time. There were always visitors from all over the world. He had a visitors book in surgery that he was proud of … people who came through signed their name and where they were from. At the time, Seattle – along with the Cleveland Clinic and Mayo Clinic – were known for thyroid. Dad made his name in thyroid surgery.
“My dad was so honest that in 1920 he wrote an article for the Journal of the American Medical Association on mistakes in 100 thyroidectomies. Think about how many doctors have written about their mistakes. He loved people. He loved to talk. He was unflappable. Something would go wrong in surgery and it didn’t bother him a bit. He’d stop surgery, turn around, wash his hands and tell a story. Then he’d come back and finish the case. He was never curt. If a resident did something wrong, he’d never call them out. He’d simply explain why it should be done another way.
“Dad was not a businessman or administrator. Had it not been for Mr. Dare Sr., I’m convinced the hospital would not be where it is today. Mr. Dare was known as the ‘no man.’ The doctors always wanted to get their money. He would say, ‘No. Not until the bills are paid.’
“At the end of their first year of business, the partners were $40,000 in the red. They didn’t have a dime. The president of Seattle Bank was Mr. Kelleher. Mrs. Kelleher happened to be my godmother. Dad went to Mr. Kelleher and said, ‘We need $40,000. You’re my son’s godfather. You’re from Virginia and so am I.’ Mr. Kelleher said, ‘I’ll loan you the money, but the partners’ wives need to sign the agreement so they know how in debt you are.’ I never saw my mom madder. But she went down and signed, along with the other wives.
“My dad’s biggest disappointment was that he never taught medical school. When he was ill in the hospital, he said, ‘I know I’ll never be able to operate again, but I’m going back to the University of Virginia to be a professor of surgery.’”
John Dare: Mason Clinic, Hospital Administrator Beginning in 1935
(Excerpted from interview by Dr. William Steenrod on Oct. 11, 1985)
“Talking about the Depression. We used to have plenty of credit problems. Patients had a terrible time paying their bills. Those were the early days of neoarsphenamine that they used to treat syphilis with. We had a rule in the clinic that you couldn’t get that treatment without paying cash in advance. It probably preserves the moral character of the individual, although it wasn’t all that good.
The physician partners had just bought an X-ray deep therapy machine. They had the only one in town for the early treatment of cancer. It cost them a lot of money. They were so wounded financially by buying this gadget, that they made patients pay for their deep therapy treatments in advance. Of course, you could come into the clinic and get any other treatment in the world on credit, but they marked out these couple of things as they needed money in advance. The Depression went on a lot longer than we all thought it might. Everything seemed unchanged up to about 1939.
The physician partners ran the clinic on a nightshift for quite a while. They were the principal doctors for Boeing in the early days, when they had an ambulance and nurse down there. We used to examine all their new hires and, in 1939 – when they started hiring by the hundreds rather than just a few – we had a heck of a problem trying to take care of them all.
We were getting five or six bucks an examination, including the lab work. They were coming in mounting numbers. So, the clinic started staying open nights in 1940 or 1941. They put on a nightshift and the physician partners would alternate coming in every third night. During the course of an evening, they would go through a couple hundred Boeing exams, do all the lab work and clear them for employment with Boeing. Although it might have killed off a few of the docs, this very unusual work was damn good financially.
Everybody took their turn. Dr. Blackford and his physician partners came down and worked nights. The sad part was that World War II was starting. Income tax started moving up fast and they probably took all the night work and gave it to the Government anyway. Boeing eventually hired its own medical staff. They had to. We got rid of the challenge.”
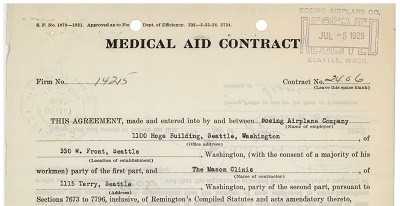
1929 clinic contract with Boeing Airplane Company
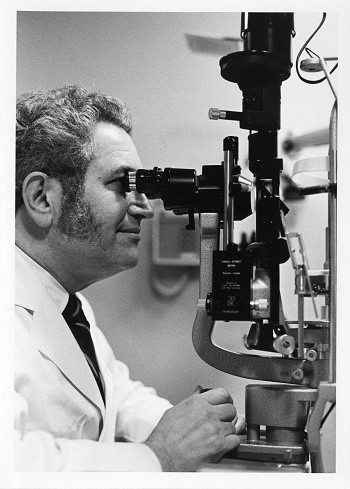
Melvin Freeman, MD: Ophthalmologist Who Started at Virginia Mason in 1979
(Excerpted from an interview on Nov. 3, 2016)
“Because my father was an optometrist, I wanted to go into the health care field. My folks told me I could go to any medical school I wanted, as long as it was the University of Washington and I lived at home. So, taking that advice, I decided to go to UW and reside at home. We lived in Montlake. So, that was an easy walk to the university. At that time, tuition was $75 per quarter, but the medical school was much more expensive. It was $150 a quarter. So, that’s why I lived at home.
In those days, you could get into medical school after three years of college, and you did not have to pick your residency until your internship year. I graduated in 1960. You had an internship, general internship and then – during that year of your internship – you actually applied for your residencies. Because of our family interest in eye care, it seemed to me that it was such a small organ I really should be able to master it. Little did I know that wasn’t true. I applied and got a very nice residency at Washington University Barnes Hospital. I was out of town for 10 years.
My first experience with Virginia Mason was in the 1950s when I was diagnosed with a heart murmur and my family doctor sent me to see Robert King, MD – a specialist in the old hospital building. I still have the note Dr. King sent my family practitioner with all the names of who were the internists at Virginia Mason, which was a very short list of four or five. Turns out, I may have had rheumatic fever as a child, but I had no limitations on my activities.
I later joined Virginia Mason in 1979. I was in Boston doing my fellowship and became interested in returning to Seattle. There were three opportunities: University, Group Health and Virginia Mason. I was out in August and had interviews with Drs. Joel Baker, John Walker, Pearson and Randy Pillow. I went over to Dr. Walker’s house for a dinner, got the flu, fainted and they revived me. I thought for sure that was the end of my career at Virginia Mason. But, no, they came in with an offer. Apparently, they must have done a complete physical on me at that time and felt I was healthy enough to work here. So, I was offered the opportunity to come here, and it was very exciting because I had two other offers.”
Why build a hospital?
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
In part, the Mason-Blackford-Dwyer Clinic group’s urgency to build a hospital was fueled by the great influenza epidemic of 1918-1919 (the “Spanish flu” pandemic), which demonstrated a serious shortage of hospital beds in Seattle. But the underlying reason was that Dr. Mason and his colleagues wanted to have the freedom to develop a new style of medicine patterned after the fast-growing Mayo Clinic in Rochester, Minn. What they planned was a combination of a privately owned hospital and a group practice of specialty trained physicians – a medical center of a scope and quality available nowhere else in the West. Group practice was frowned upon by traditional physicians of the time. In those days, it was only acceptable for physicians to be in solo practice.
The hospital they envisioned would house modern laboratory and X-ray facilities, surgery and delivery rooms as well as sufficient space for 80 inpatient beds. The main floor would have private offices for clinic doctors. The whole organization would be operated under joint management of the clinic and hospital.
Months before, in discussions with his friend, Dan Kelleher, president of the Seattle National Bank (later Seafirst and now Bank of America), Dr. Mason had revealed his idea of the combined hospital and clinic facility. Kelleher replied, “Go ahead, Tate. I will see you through,” which was a statement that would prove to be prophetic.
The dream began to take form from there. Plans were developed in 1919 and the hospital site was chosen. A corporation was formed and bonds were purchased by clinic doctors and others, which provided money to begin construction.

Anonymous
Virginia Mason Seattle
“In October 2015, I was admitted into the Emergency Department with a .39 BAL (bioartificial liver). A severe, late-stage alcoholic at the age of 36. In full restraints (which was necessary after an attempt to run), one of the patient care technicians (PCT) was assigned to sit watch at my door. During my stay, she talked to me, not at me. She didn’t judge me. She got to know me as a person, not an addict. Turns out she was the mother of one of my son’s friends, who had spent many after-school hours in my home. She volunteered to work a double shift so she could stay with me. She arranged for my friend, who was a new mom and nursing, to have access to a breast pump. When my friend realized she had taken the car keys with her, leaving her husband stranded without car seats for three kids, my PCT drove to my friend’s house and dropped off the keys at the end of her shift. The kindness, compassion and understanding she gave has stayed with me. She is a part of my journey into a life of recovery where, in October 2019, I will celebrate four years clean and sober. When I was at my jumping-off point, as low as I could get, she showed me grace and compassion.”
Melissa Jackson Witek
Virginia Mason Bainbridge Island, Virginia Mason Kirkland and Virginia Mason Seattle
“Late at night and with our 10-month-old daughter in tow, my husband rushed me to the Virginia Mason Emergency Department on First Hill in Seattle. I had just been told by my optometrist at Virginia Mason Kirkland, who I had seen for a retinal hemorrhage, that my blood work indicated I had leukemia. I was in acute distress and had serious symptoms related to an extremely elevated white blood count. Sometimes the best things happen at the worst of times. Dr. David Aboulafia happened to be the oncologist on call that night. That was almost 20 years ago. With kindness, a gentle bedside manner, and a medical knowledge beyond compare, Dr. Aboulafia has seen me through a bone marrow transplant, several serious post-transplant infections and complications, five joint replacements, several eye surgeries, and the long-term side effects of my treatment. He has coordinated my care with other Virginia Mason departments, as well as with the Seattle Cancer Care Alliance, where I had my transplant. I remember a nurse in the Emergency Department that night telling me that my baby girl was my reason to live. Because of Dr. Aboulafia and great care from the entire team at Virginia Mason, I am excited to celebrate my daughter’s 21st birthday with her later this year!”
Medical Advances Involving Large Mammals
(Excerpted from “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”)
“In 1934, Virginia Mason’s Bob King, MD, teamed up with Paul Dudley White, MD – a physician from Harvard and President Dwight D. Eisenhower’s cardiologist – to perform the autopsy on ‘Tusko,’ an elephant at Woodland Park Zoo.
“Years later, the two research partners joined up again in the Bering Sea, where they conducted the first cardiogram on a whale.”
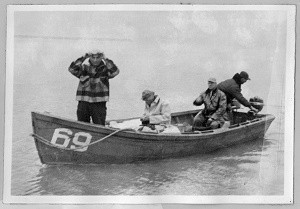
1952 “Whaling expedition” including Drs. Robert King and Paul Dudley White.
Robert Mendoza, PCT: Good Care Begins with Trust
(This team member profile article was originally written for posting on Virginia Mason’s intranet, V-Net, in April 2015.)
Listing the duties of a Patient Care Technician (PCT) would fill a notebook, and yet no regular job description would capture what Robert Mendoza, PCT, brings to his patients. There is assisting with treatments, medications, checking vital signs, help with transferring, personal care, and ongoing documentation, just for starters. But for Mendoza, there’s something else needed in the mix: a patient’s trust.
“I like to build trust with my patients through communication,” said Mendoza. “Connecting with them in conversation or with laughter helps patients feel comfortable with me and what I’m doing.”
Mendoza knows that trust also comes from a patient’s confidence that help will be there when they need it. He visits his patients regularly without waiting for the call light, asking if there’s anything he can do. Mendoza can tell when a patient is distracted, sometimes by pain or anxiety, and might not be aware of their own needs. That is when he will suggest something – a different position or a warm shower, perhaps – that could help them feel better.
“Sometimes what they need is for someone to listen,” said Mendoza. “There’s no medication that can help with that. So, I stay and talk with them.”
Since even routine patient care, like getting vital signs, can feel invasive, he makes sure to describe step-by-step what’s happening. It is one way to show respect for his patients, as he tries to put himself in their place. Having empathy for his patients comes naturally to Mendoza, which he attributes to loving what he does. One of the biggest rewards he says is seeing people get better.
“I give my patients quality care and a good patient experience because I work from my heart,” said Mendoza.

Robert Mendoza, PCT
Jerry Sluman: Grateful Kidney Transplant Recipient
“After steadily watching my kidney function decline over the course of seven years, I was informed that I was ‘running out of runway.’ My kidneys had officially failed. It was time to swallow my pride, share my story and search for a living donor. After persistent campaigning, I was lucky enough to have 30 people go through the donor screening process. Of those 30, three were potential candidates. Of those three, there was one exceptionally matched friend. His name is Brock Sabo and he was generous enough to donate a kidney to me. Our surgeries took place at Virginia Mason Hospital Aug. 7, 2018.
“Everyone at Virginia Mason took outstanding care of both Brock and I. This includes Nephrology, surgeons, nurses, therapists, dieticians, social workers and every other team member who took part in our successful care.
“I couldn’t imagine receiving better care across the board and am extremely grateful.
“A special thank you to all the special, empathetic people who helped me through the process to achieve a second lease on life – especially Virginia Mason team members, Brock and Sarah Sabo, Jodi and Patti Baker, Kristin Henderson and Ryan Aal!
“Happy 100th birthday, Virginia Mason. Keep up the great work!”

Kidney transplant recipient Jerry Sluman (left) with his friend and living donor, Brock Sabo (right).
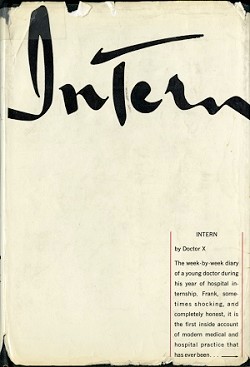
Best-Selling Book in the ‘60s Described Experience of a Virginia Mason Intern
(Excerpted from the book, “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”; Written by Charles Hammer, MD)
“In July 1960, Alan Nourse, MD, who had been an intern at Virginia Mason in 1955, published his book, ‘The Intern,’ under a pseudonym (Dr. X). This national best-seller was a thinly disguised account of his experiences as a housestaff officer at Virginia Mason Hospital.
“Dr. Nourse assigned pseudonyms to many of the active partners in the Mason Clinic, but his descriptions of the characters were so accurate that we could easily tell who was who.
“At times, the person portrayed would deny that he was the character in the book (especially if the description was not particularly complimentary), but the rest of us knew who was who.
“In truth, the most disappointed partners were those who could not find their resemblance in print.”
“The real story of how the hospital was named,” according to Virginia Mason Blackford Morris
Miss Virginia Mason raised Virginia Blackford’s grandmother, because her grandmother’s mother had died; Miss Virginia Mason was her grandmother’s aunt.
When John Blackford was born, it was not considered proper for “the boys” to potentially “hear something” related to a woman in labor. So his mother was put in a carriage and driven 2 miles down the road to Miss Virginia Mason’s house, and that’s where he was born.
Later he roomed with her while at the University of Virginia; she ran a boarding house for medical students. So, as his great aunt, surrogate grandmother, she had a great bearing on his life, and his mother’s life, which is why he named his daughter after her, Virginia Mason Blackford.
When the two mothers, Mrs. Tate Mason and Mrs. John Blackford, were together one evening while the doctors were down polishing the floors before the hospital opened, they were discussing what a coincidence it was that there were two girls with the same name. (The other Virginia Mason was supposedly named after the state of Virginia.) So the two mothers decided this would be the perfect name for the hospital.
Recorded Sept. 25, 1996 with the Virginia Mason Historical Society.

Injured Policeman More than Doubly Fortunate
(This article was originally written for the October-November 1975 issue of Pulse, Virginia Mason’s employee newsletter.)
When Officer Tyrone Sheffey was injured in the line of duty, he had cause to thank his lucky stars, more than once over.
Being sped to the new Virginia Mason Hospital Emergency Service Department was one. Listed in satisfactory condition was another. But most fortunate of all is that Mrs. Claudia Mitchell, LPN, works here. Why? She is part of his family, his wife’s mother. Mrs. Mitchell stayed with Officer Sheffey the night he spent in Special Care and was close at hand throughout the remainder of his stay.
Sept. 7, 1975, was a day Mrs. Mitchell, a Virginia Mason Hospital employee of 14 years, vividly recalls: “My daughter called after a couple of police officers came to her house. She said she was bringing the children over because something had happened to her husband. After she hung up, I immediately called the Emergency Room, and they told me his condition was satisfactory. After we arrived at the Emergency Room, we saw he was in pretty good spirits. But we were just numb.”
“They let me stay with him all night in Special Care. He said later that he knew I was there and held his hand while he slept.”
Officer Sheffey is home and doing fine now. He does, however, have one problem of serious proportion, responding to the many friends and fellow officers from all over the state who deluged him with cards, flowers and get-well-soon messages.
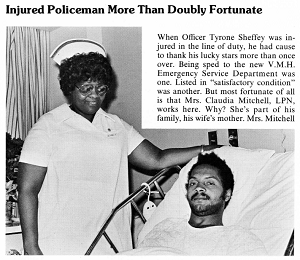
Mrs. Claudia Mitchell, LPN, with injured Officer Tyrone Sheffey. Mrs. Mitchell is also Officer Sheffey's mother-in-law.
Robert King, MD: Began Practicing at The Mason Clinic in 1931
(Excerpted from an interview by William Steenrod, MD, on April 11, 1985)
“Dr. John Blackford, brother of Stage Blackford, who was instructor in internal medicine at the University of Virginia, encouraged me to come out to Seattle. I went to Clifton Springs Sanatorium and was offered a job there for $3,500 a year. But due to my father's persuasion, I came out here because he thought going to New York was like going to the land of the living dead and, out here, there was considerable opportunity.
I had an uncle who had spent time in Alaska managing a gold dredge in Nome on the Snake River. In the winter, he would spend time in Seattle. He knew Seattle well and was a patient at Virginia Mason Hospital. He also encouraged me to come to Seattle. I was in correspondence with Dr. Blackford and then Drs. Joel Baker and Louis Edmunds wrote to me. I finally came out. I became a staff physician at The Mason Clinic in June 1931.
We were paid $250 a month. We furnished our own car, made house calls and worked in the office. At the end of 1932, I was still making $250 a month. Thankfully, I received a raise to $300, but then my pay was lowered by 20 percent to $240 per month.
We used to borrow $10 from one another to get through the month. Dr. Edmunds was married at the time and was having a little harder time than we were. I went to live with Dr. Baker in a bachelor establishment here in Seattle, called the Hacienda. Drs. Baker, Wilkinson, Edmunds and I took turns making house calls.
Dr. Blackford was the reason I came to Seattle. He took me under his wing professionally and socially. I used to have Sunday dinner at his home almost every Sunday. He and his wife were extremely nice to me. I felt very close to him. He was almost a genius from the standpoint of sizing up a situation. He had a strong feeling for patients’ emotional disturbances. Sometimes, he would spend two to three hours with a single patient, while keeping everyone else waiting. He smoked like a chimney – about 50 to 60 cigarettes a day. He used to carry packs of 50 in his pockets. He was also a boat lover. He spent a lot of time on his boat. However, he gradually developed emphysema and a cough. Sometimes, he would start coughing so hard that he would produce superior vena caval obstruction, resulting in a spasm.”

Robert King, MD
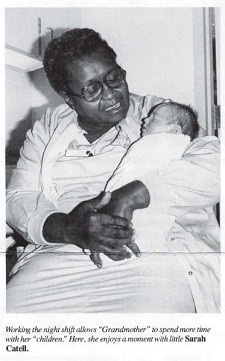
A Notable Nurse: Louella Jackson, LPN
Louella Jackson, LPN, retired from Virginia Mason in February 1989. She was known to staff and patients as “Grandmother” and had the practice of calling babies in the nursery her children. She worked at Virginia Mason from 1966 to 1989.
Don Olson: Virginia Mason Administrator Starting in 1965
(Excerpted from “VMMC History – Reflections by Don Olson,” and an interview by David Wilma on June 1, 2018)
“When I was working for M.D. Anderson and Tumor Institute in Houston, I heard John Dare of Virginia Mason Hospital and The Mason Clinic was looking for an assistant. I had been to the Seattle World’s Fair and decided that if I ever got the chance to live in Seattle, I would grab it. I called John Dare and introduced myself. After interviewing with him, he gave me the job as assistant administrator of The Mason Clinic. We arrived in Seattle on July 12, 1965 and I retired in 1998.
“My arrival at the Virginia Mason Hospital and Mason Clinic found three separate organizations all closely linked. The Mason Clinic was a partnership and the hospital and research center were nonprofits. The heart and soul of the hospital was The Mason Clinic. There were 55 physicians, including the partners and soon-to-be partners. It’s hard to imagine, but for the annual Christmas gathering, we all had dinner at one long table inside Broadmoor Country Club.
“There were no computers to support patient billing. So, we had thousands of pieces of paper that came from physician offices, laboratory, radiology and any other point of patient care service. This paper jungle nightmare was represented in buckets of ledger cards that reflected each patient’s account. Soon after my arrival, we began the process of converting to the IBM punch cards.
“Virginia Mason was a family. Everything operated from the ground up. Patients were the focus and team members who were closest to the patient were the hierarchy. What we excelled in was exquisite patient care. There isn’t anything that goes on in the hospital that nurses don’t know about. If you want to run a good hospital, you’ve got to speak with nurses.
“I never had a bad day there and never had a day go like I thought it was going to go. I was surrounded by very gifted people. We were all pulling on the same rope. Wherever you went around the state, you would bump into people and they would say, ‘You work at Virginia Mason? Oh, my goodness.’ Then, they would tell you their story about how well they were cared for at Virginia Mason. In my era, there we were going into a new age of sophistication, but Virginia Mason had the cards.”
Thomas Green, MD, Orthopedic Specialist
(Extracted from an interview on Oct. 20, 2016)
“I started practicing at The Mason Clinic in 1975. There have been a lot of changes in imaging that have made a big difference in medicine. The most significant one was probably digital X-ray. Obviously, CT scans and MR technology have revolutionized the way we see things. Our ability to quickly move images – as well as view and refine them on a digital framework – was a big improvement that came when we moved into Lindeman Pavilion. Arthroscopy was also a huge change. That was sort of the beginning of outpatient surgery, where you could do significant procedures and people would return home the same day. When I came to Virginia Mason, arthroscopy cases were not being done. So, I started doing them myself. I didn’t have a fellowship or special training, just what I learned from my professors at the University of Washington Medical School.
As a result, I was involved in buying our first arthroscopes for the operating rooms. Don Verg, who was an administrator in Acquisitions, asked me, ‘Do you think this will ever be used enough to justify it?’ I looked at him and laughed. Today, endoscopes are likely the most universally used pieces of equipment in operating rooms, other than maybe pickups and scalpels. Now, my general surgeon colleagues use endoscopes and arthroscopes all the time. The first arthroscopes were modified cystoscopes. They just used a different mechanism to shorten the piece inside.
One of the things I particularly liked in my years at Virginia Mason, was the way the clinic helped facilitate physicians’ care of patients. It was very helpful and appreciated.
If you had a challenge and were not sure what to do, there were always people around to help resolve issues and get things back on track, so patients were taken care of properly.”

Peggy Nystrom
Virginia Mason Seattle
“I was born at Virginia Mason in 1945 and both of my children were also born there. The first on April 27, 1966 and the second on Oct. 24, 1969. The same doctor who delivered me, Dr. Rutherford, also delivered my two sons.”
Jessica Entz
Virginia Mason Bellevue, Virginia Mason Federal Way and Virginia Mason Seattle
“I have been coming to Virginia Mason for more than a decade. I am honored to say that it is my home away from home. I have had multiple sclerosis since I was in eighth grade. Dr. Kita and her staff are like family to me. I trust them with my life. Her knowledge and commitment to me – as a patient, granddaughter, daughter, sister, niece, cousin and friend to many – means so much!”

Virginia Mason’s Development of Satellite Clinics
(Excerpted from the book, “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”)
“As part of a medical staff retreat at Alderbrook Inn on Hood Canal in February 1980, a special report from an ad hoc committee focused the group’s attention on what was to be a major strategy change for the clinic. The decision was made to experiment in the primary care satellite field. The first tenuous move came with the development of affiliation agreements with clinics in West Seattle and Friday Harbor. The medical center entered the field more seriously through the acquisition of Dr. Wes McElroy’s practice at his clinic on Highway 99 near Sea-Tac Airport, where Dr. Ed Meyer served as the first clinic physician to practice away from the main campus. The arrangement lasted for only a short time.
“On Sept. 8, 1980, in a memo to Bob Webb, MD, chairman of the Ad Hoc Committee on Satellite Clinic Development, Dr. Bill Steenrod noted, ‘It seems to me that the only reason to go into the satellite business is eventually to develop into an HMO or whatever the catch phrase is at the time.’ He went on to say, ‘What we are trying to determine at present with the first satellite is whether or not this first step and subsequent ones are bound to land on banana peels.’
“But satellite clinics were in the future. The decision was made to move forward in the summer of 1980and land was acquired adjacent to Evergreen in Kirkland for a new clinic to be called Mason Clinic East. As competition in health care became an accepted fact and routine occurrence, clinic operations were subsequently established in North Bend, Mountlake Terrace, Alderwood Mall, Issaquah, Redmond, Bellevue and Federal Way.
“Much was learned during those years about how to manage separate clinics. One lesson was that systems designed for a large downtown facility did not necessarily work at a branch clinic. Adjustments had to be made. Physicians who practiced in branch sites and their downtown colleagues had to learn how to relate to one another. Bob Webb, MD, was the first clinic physician to operate out of Mason Clinic East and he was joined by Gary S. Kaplan, MD, in 1983. Gary had completed his residency in internal medicine at Virginia Mason, knew the medical center well, and had a great enthusiasm for the development of satellite clinics. He later headed up the entire clinic satellite system.”
Louis Edmunds, MD: Started Practicing Medicine at Virginia Mason in 1928
(Extracted from an interview on April 16, 1985)
“I graduated from the University of Virginia in 1928 and was looking for a job. UV offered me an internship, but they only offered room and board with no salary of any kind. I needed something besides room and board. I finally received an offer from Virginia Mason with room and board plus $50 a month. That offer made the decision for me. I was also given expenses for the trip out and back. So, I travelled to, and arrived in, Seattle on July 1, 1928.
Dr. Bob King also came out to be interviewed and look over The Mason Clinic and he has been here ever since. Then, my sister came out to visit me, met Bob and they now have 17 grandchildren and counting.”
[Margaret Edmunds, Louis’ wife: “I’d like to add something to Louis’ story. They may have given $50 a month to the interns. But, some way or other in the first week – with all their card games – the $50 moved around. When things were really bad, they sold their tickets back home. They were stuck.”]
“We did a lot of State Industrial insurance work and what we called ‘steamship cases’ that came under the longshoreman’s workman’s compensation. Mason Clinic did get into a little trouble with the King County Medical Society. Dr. Mason was quite a go-getter, you might say, in getting business. He signed a contract with the police department to furnish medical care to officers. I forget how many policemen we had then, but there were quite a few. They had contracts with the steamship companies, The Boeing Company and the Postal Service. Because of this so-called ‘contract medicine,’ the Medical Society stated they were going to kick us out of the Society if we didn’t give it up. It has always amazed me that around 1932, the clinic was threatened with expulsion from the King County Medical Society and, four years later, Dr. Mason was president of the American Medical Association.”
[Margaret Edmunds: “Few people could resist liking Dr. Mason. He had a winning personality. When he talked with you, you felt you were the only person on earth he was talking to. Absolutely wonderful. He charmed everyone.”]
“Dr. Lester Palmer was interested in diabetes. He trained under Dr. Elliott Proctor Joslin, the first U.S. physician to specialize in diabetes. He also promoted diabetic camp for Boy Scouts and Girl Scouts. Dr. Palmer always took a nurse to camp with him to administer insulin, etc. I think he probably paid for all of this out of his own pocket. Lester was the camp doctor and Margaret Brown was the nurse there for a number of years. He later formed The Diabetic Trust Fund between 1938 and 1939.
I was in the lab doing blood sugars on all these little diabetic children when I said to Dr. Mason, “These are the healthiest children I’ve ever seen. Is there something about diabetes that makes their cheeks so rosy and look so well?” He said, ‘No, it’s just the careful care they’ve been having.’ These children looked wonderfully well.”

Margaret Edmunds: Wife of Dr. Louis Edmunds, Hospital Employee in the ’30s
(Excerpted from an interview with Margaret Edmunds and Louis Edmunds, MD, on April 16, 1985.)
“We were married in 1930. I started in January 1929 and worked until 1931. I was pregnant and in those days you didn’t work after you were pregnant. Mr. Gibb was in charge of the laboratory. I came to ask if I could work 15 hours a week with no pay. It was for credit at the University of Washington. I had to have two quarters, five hours each, of practical experience to get my degree in bacteriology. I applied here. They sent me to Mr. Gibb. The first thing he asked me was, ‘Do you know German?’ I said, ‘Yes.’ He didn’t ask me another question. He was working on his master’s, and he couldn’t read the German textbooks he had to read. So, every day, I had to read a little German to get him through. That is one way to get a job. After those two quarters for credit, they offered me a job.
I would work in the lab from 7 a.m. to 8 a.m. and draw blood from 5 p.m. to 7 p.m. They gave me room and board and I was thrilled since I was going to be working with patients. I had all my meals there. The dietitian was Louise Powley, who always had a student intern with a bedroom in the nurses’ home. The boy who ran the switchboard at night was a student at the University of Washington, so he gave me a ride to campus and I took the trolley back down.
The laboratory was in one little room, opposite the X-ray. When the interns were moved to the little cottage on the lawn, their quarters were turned into the lab and that was a great expansion for us. The farthest room was pathology, and then they had blood chemistries and Wassermans in the middle room, and the general room for blood counts, urinalysis, etc. One patient room and a room for storage.
I think another reason the clinic has prospered is that all of the members in the beginning were generous. Nobody was criticizing. They were working together as a group. I was working in the lab and had to do a c02 examination. We had an instrument that had mercury in it. You had to let the mercury out very slowly or it would break if it popped up too fast. It cost $8 to get one of those. I had this test to do and I broke it. I got all my courage together and went into Mr. Dare and told him I had broken the equipment. He told me that was OK. I went back to the lab and broke a second one. I thought I had better resign and go home. I offered to pay for it. I couldn’t think of anything else to do. Never a word of criticism. Just always generous, always so nice. I think that spirit went throughout the clinic. Doctor Mason was that kind. They were nice to everybody.
The partners always looked forward. I don’t think they ever said now we are big enough. I think they never even considered it. We need another man, we need another this. This department needs help. They also always encouraged writing and research.
When I was in the hospital for two weeks a couple of years ago, the thing that impressed me was the courtesy and generosity of the nurses to each other. I never heard an unkind word said between the nurses or anyone else. I think it is amazing. I wrote a little note to Don Olson afterward because I think that takes a lot of planning when you get the spirit throughout an institution. It was there in the beginning, too. It was a happy place to be!”

Margaret Edmunds with husband Louis Edmunds, MD
Keith Lundberg: Former Virginia Mason Administrator Left His Mark
Keith Lundberg was an integral part of the Virginia Mason team for 20 years. During his tenure, Lundberg served as director of the Health Services Consortium and as associate administrator responsible for regional and international relationships.
In 1987, Lundberg said, “The Health Services Consortium gives regional health care providers in a highly competitive field the opportunity to cooperate with one another in delivering coordinated health care to all of their patients.”
In 1988, he was appointed to the National Advisory Committee on Rural Health Policy within the Health Resources and Services Administration in Washington, D.C., and served in that position until 1993.
He was dedicated to improving patient service by applying telecommunication technologies to improve access to health care services. Leading an effort to expand accessibility of specialty care to remote hospitals in Washington state, Alaska – and even the far east region of Russia – Lundberg was instrumental in promoting the first telemedicine program in the region at Virginia Mason in 1995.
The Keith R. Lundberg Media Center is the base site for Virginia Mason’s telemedicine programs in Volney Richmond auditorium on the main campus. Virginia Mason’s Regional Clinicians Program also sponsors the annual Keith Lundberg Lectureship, which has honored Lundberg’s championship of regional and international clinician relationships since 2006.
When Lundberg left Virginia Mason in 1998, he developed a consulting business, Medical Resource Strategies, working with various businesses and organizations interested in innovative communication techniques. In 2001, he was awarded the Joe Hopkins Award by the Washington State Hospital Association for his dedication, leadership and influence on the hospitals of Washington state.
Unfortunately, Lundberg died in 2002, after battling leukemia. He was 55. He was known as a man of integrity who loved his family and supported the community. Lundberg was survived by his wife, Sally, along with a son and daughter.

ChapStick Search for a Head of State
(Excerpted from the book, “Vision and Vigilance: The First 75 Years: Virginia Mason Medical Center, 1920-1995”)
“In 1993, Virginia Mason was selected to provide emergency medical care for President Clinton and other heads of state attending the Asia Pacific Economic Cooperation (APEC) conference in Seattle.
“John Ryan, MD, chief of surgery, was named to head the Virginia Mason medical ‘SWAT’ team, which anticipated every contingency. Dozens of providers were on call and Dr. Ryan and others accompanied the principals at every function, including the big wrap-up conference held on Blake Island, where everyone arrived by boat. A flotilla of craft filled the dock area.
“Suddenly, a call for medical care came in. One of the heads of state needed ChapStick. While the medical chests were fully provisioned with every possible emergency and tertiary care supply imaginable, no provision had been made for chapped lips.
“Drs. Ryan and Quigley initiated a search and located one partially used package on one of the boats. It was formally presented on a tray to the chief of state by his assistant – and rejected. The search continued until an unopened package was located on one of the anchored boats.
“Virginia Mason, prepared for specialty and tertiary care, carried the day again with its persistent search for the non-prescription item. The outcome of the conference might well have been jeopardized by chapped lips.”
Needs of the patient must always come first
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
There is a story about Virginia Mason co-founder James Tate Mason Sr, MD, that was passed down through the hospital’s administrative ranks over the years. Dr. Mason allegedly kept a jar of pennies and other change on the mantle of his fireplace at his home in Black Diamond, Wash., where he was employed as the doctor for a coal company at age 25 between 1907-1909. The jar contained some of the money local coal miners and their families had paid him for taking care of them. He kept the jar there as a reminder of just how poor and needy some of his patients were. The message to administrators was that the needs of the patient must always come first and that “pocketbook needs” are secondary.

James Tate Mason, MD
Pam Salvatore
Virginia Mason Seattle
“Dec. 4, 1986 was a popular day to have a baby! When I showed up at 2 a.m. at the front desk of Virginia Mason’s delivery unit, I was breathing hard and in active labor. I soon learned that every birthing room was occupied. There were no empty beds! This was a problem since I was 9 cm dilated and well on the way to having my first baby. Thanks to some quick, creative thinking by the nurses, a convertible chair-bed was moved from one of the birthing rooms into the unit’s linen room, which was transformed into my own personal birthing suite. At first, I was disheartened that I wouldn’t get to enjoy a Jacuzzi tub or birthing bed that I had seen during my pre-birth tour several weeks earlier. But as I got settled into the linen room, I was surprisingly comforted by my surroundings. All around me were crisp, white, clean linens – towels, washcloths, sheets and blankets – all neatly folded and stacked, unlike the ones in my home. I felt very safe, cozy and comfortable amidst all those linens. But the most wonderful thing in laboring away and giving birth to my son in that linen room was the view from its window. I had a clear view of The Bon Marche’s holiday star, which was illuminated on top of the building, as well as a view of the neon “S” on top of the Sheraton Hotel. Together, they provided the best focal points I could have imagined. When my son was born, I named him Sam and gained a wonderful story to tell him of how he was born in a linen room with a view of the holiday star and the first letter of his name. I couldn’t have been happier!”
Hugh Jones, MD: Mason Clinic Pathologist Starting in 1949
(Excerpted from an interview with Hugh Jones, MD, on June 13, 1990)
“It all started at Walter Reed General Hospital, where I was chief pathology and underpaid by the armed forces, with six children. We decided that I had to get out of the service and into a job where my income would be higher. I resigned from the service and put out feelers for positions in pathology. Through a mutual friend, Dr. Stewart, who director of the National Cancer Institute in Washington, D.C., I learned that Dr. Baker was looking for a surgical pathologist at the Mason Clinic.
I received a letter of inquiry from Dr. Baker in November 1948 asking if I would be interested in coming to Seattle and offering to pay for half my travel expenses so I would be spared any embarrassment, lest I not accept the position. So, I came to Seattle, met Dr. Baker and was royally cared for in his home. I also met members of the clinic, saw the facilities and spent half a day with John Walker, visiting with him and seeing the construction on his new home in Bellevue. After some thought, I accepted the position and arranged to rent a house for my family.
On Jan. 1, 1949 we arrived in a Seattle snowstorm after driving across the country in a station wagon with my wife and six children. We were fortunate to have very generous and fine landlords, who arranged for us to get a check cashed when we arrived and had the house warmed and ready for occupancy.
The hospital’s clinical laboratory consisted of a small area that was probably 50’ by 75’ feet. Hematology was also very small and bacteriology was a closet. Regardless of size, it was well run. Eleanor ran that place and she was Mayo Clinic-trained. She was a very fine supervisor and could do anything. She could perform any of the tests in the lab.
We had a little beef with City Light because the power was not clean. The man came out with a multi-meter and said it looked fine. We were never able to get good, clean power in that lab. We always had surges, which didn’t allow us to use any amperage. We had a glitch every time Bethlehem Steel turned on their furnaces. So, we eventually went to batteries.
Joe Crampton was really a visionary in the clinic at that time. He and I often spoke of an organization, which would bring together quality physicians at the clinic with basic research staff. We felt that, together, we could really produce some meaningful research. Joe outlined his ideas about such a research center in writing. At the request of the clinic partnership, Joe and I drafted a document that better defined what we were talking about. It was accepted and presented to the partnership for approval. The partnership unanimously approved the principle and authorized us to seek out a scientific director for research.
I have felt that immunology was an area we could probably contribute more from our clinical materials than almost any area that I knew.”
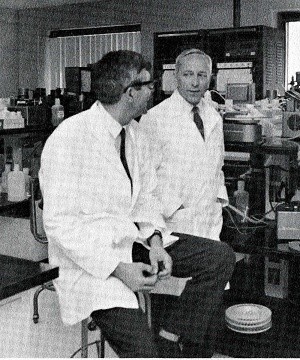
First Superintendent Remembers when Virginia Mason Opened in November 1920
(Excerpted from “History” by Anna Fraser, RN, 1927)
“Virginia Mason Hospital opened Nov. 1, 1920 at 8 a.m. and from then until 5 p.m. that day visitors were received for an inspection of the new building. In the evening, the first patient arrived with a nurse to care for her and the following morning the first operation was performed by Dr. E. E. Grant.
The staff, which opened and carried out the first services of the hospital, consisted of the superintendent, Ms. Fraser, two surgical nurses and a dietician. But, from this nucleus, a compact organization was soon formed. The dietician, Ms. Fulford, promptly engaged two cooks who, in turn, employed the necessary kitchen assistants. Two janitors were also hired. Among their first duties was arranging furniture in the rooms and they were ably assisted by the doctors. The doctors proved to be very versatile in those early days of adjustment. At odd times and in odd places, they might be found vigorously scrubbing the floors, apparently thoroughly enjoying an hour of muscular recreation.
Among the major adjustments during those first days was the matter of the wrongly placed switchboard. It was supposed to be installed in the hospital office but, for some reason, it was put in the clinic. The resulting inconvenience – even disaster – can easily be imagined. So, there was only one telephone connection in the hospital office! It resulted in running up and down stairs and mix-ups in telephone messages. But this, like all things, soon passed. The switchboard was eventually installed in its proper location inside the hospital office.”

Julie McAferty
Virginia Mason Seattle
“I started working at Virginia Mason in 1989 as a newly graduated RN and loved it. I really appreciated all my mentors and have many great memories of my time there. One very memorable experience occurred when I was involved with a c-section as a night-shift circulating nurse. As I helped the patient recover, my contractions began getting stronger. After finally telling my co-workers, I was admitted at 5 cm dilated and had my baby before the end of my shift!”
Racing to catch a ferry
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
“One story about Dr. John Blackford was the afternoon he was racing down Seneca Street to catch a Puget Sound ferry. He noted that the car behind him was also going very fast. Dr. Blackford figured that the car behind him was trying to catch the same ferry. Once onboard, Dr. Blackford, as a Good Samaritan, persuaded the ferry attendant to hold the ferry for the arrival of the car behind him. The car boarded and a Seattle Police officer got out and ticketed him for speeding.” – Thomas Carlile, MD, emeritus physician (radiology) and past president of the American Cancer Society

John M. Blackford, MD
Tucker the Turtle: Hyperbaric Medicine Helped Heal Him Before Returning to the Ocean
(Excerpted from follow-up coverage in The Seattle Times; Sept. 29, 2017)
“Perhaps turtles are not as cute and cuddly as some animals, but the tale of Tucker the turtle’s travels is a spirit lifter.
“The turtle, who was brought to the Seattle Aquarium near death a year and a half ago, suffered from a host of problems and became the first non-human to be treated in a hyperbaric chamber at Virginia Mason Medical Center.
“But earlier this month he was released, along with two other turtles, into the ocean waters off the coast of San Diego. And since then he, and his two female companions – who were all tagged so that researchers could track their travels – have made it down to Mexico.
“Tucker was found sick and dying on the Oregon coast in 2015. He was so sick that the only way people knew the olive ridley sea turtle was even alive is that he tucked his tail in when touched, hence his name.
“Tucker was brought to the Seattle Aquarium, Washington state’s only turtle rehabilitation facility, after folks at the Oregon Coast Aquarium first found him.
“On top of his various maladies, Tucker was also suffering from buoyancy problems because he had micro-bubbles of air in his tissues (decompression sickness or ‘the bends’), which his trip to the hyperbaric chamber eased.
“He was then transferred to SeaWorld in San Diego, where his stay in a bigger pool gave him the chance to dive deep and helped him recover.
“Before his release, researchers installed trackers on Tucker and two female companions so their travels could be watched. The females had also been at SeaWorld and were ready for release.
“Tucker, who is an active and energetic youngster between 10 and 15 years old, appears to be safe and sound and doing exactly what his caretakers hoped he would do. Over time, SeaWorld staff also hope Tucker fertilizes some eggs and contributes to his species.”

Tucker the Turtle
A. Stephens Graham, MD: Interned at Virginia Mason in 1925, 1926
(Excerpted from “Reflections” by Dr. Graham circa 1982)
“My most cherished honor was the appointment by the Dean of the University of Virginia Medical School – along with Julian Coleman, MD – as the first interns of Virginia Mason Hospital. Acceptance was somewhat of a gamble. All we knew about the place was that Minor Lile’s father had been dean of the Law School, John Blackford’s father was a founder and longtime headmaster of Episcopal High in Alexandra, and his brother was my classmate.
On New Year’s Eve 1924 in New York City, I had just been appointed one of the eight interns for St. Luke’s Hospital, one of the most sought-after internships in the country. But I was ranked number eight and missed out on one of the four surgical places leading to a residency. Just a month before, I received an offer for a prestigious appointment to the Marlborough Service of Dr. Warfield Longscope of Johns Hopkins.
Bewildered and uncertain, I received a call from my classmate, John Blackford’s brother, urging me to accept the appointment in Seattle. In my frustrated state, I accepted and have never regretted it.
From the very beginning of the internship, we realized how fortunate we had been in accepting appointments. In addition to Dr. Mason Sr. – who, on the first day insisted we address him as ‘Tate,’ not even ‘Dr. Tate’ and became my immediate idol – we were tremendously impressed with John Blackford, Minor Lile, the Dowlings, Lester Palmer, Pius Rohrer, John Dare Sr. and Ms. Fraser. For many years, they became the prototype by which we judged the efficiency of other hospitals and nursing service administrators – even during the 17 years I served as vice president and chief of surgery in a private hospital.
Interesting experiences
Incomprehensible in a city of 340,000, Virginia Mason and the considerably larger Sister’s (Providence) Hospital had never had an intern and the remaining three or four hospitals had extremely few for a city so large. The doctors on staff were at a loss for how to use us. Only Pius Rohrer, MD, had been exposed to a residency in recent years and his was wholly unconventional.
We made certain suggestions and explained that we were trained to carry out nights and weekends, lab studies, including blood chemistry, Wassermans, X-rays, give nitrous oxide, ether, perform spinals, transfusions, undertake deliveries – if labor was precipitate and a responsible physician was not available – and were avid performers of autopsies.
Amazed and delighted that they could avoid the expense of technicians – along with nights and weekends – they let us work out the details. We alternated weeks for covering night calls. With Mr. Dare’s blessings, the man ‘off’ could moonlight on the Doctors Exchange for house, apartment and hotel calls. Interesting were calls directed to Virginia Mason from neighboring apartments maintained by tycoons for their mistresses, of which there were quite a few directly across from the hospital. In lieu of fees, we received tickets to shows, games and premium distilled products from Canada.
It has been a delightful nostalgic journey back to one of the happiest periods of my life. Crystal clear in my mind are many more interesting, often exciting incidences, including itinerant surgery in distant small towns; chauffeuring Tate and the operating room crew in his huge Lincoln; and dramatic, life-saving emergencies to out-of-the-way places in dense fog.”
A. Stephens Graham, MD
Virginia Mason’s Short-Lived Heliport
(Excerpted from the book, “Vision and Vigilance: The First 75 Years; Virginia Mason Medical Center; 1920-1995”)
“In the late 1960s, a heliport was built on top of the east wing of the hospital, but was short-lived.
“It was seldom used and for good reason. An adjacent elevator tower caused unpredictable air currents. When a helicopter landed, it was an event watched by many – including area residents – with some anxiety. One day, a large Coast Guard helicopter came by to try out the pad, and when it touched down, its three wheels were only about a foot from the edge of the pad.
“A management decision was quickly made that Virginia Mason should, instead, support the heliport at Harborview Hospital. Shortly thereafter, the Virginia Mason pad was quietly whisked away.”
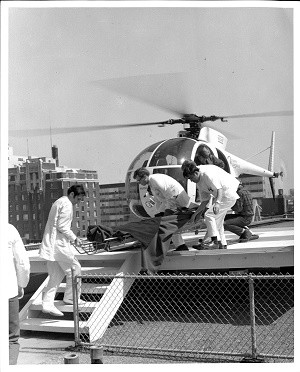
Virginia Mason’s Short-Lived Heliport
(Excerpted from the book, “Vision and Vigilance: The First 75 Years; Virginia Mason Medical Center; 1920-1995”)
“In the late 1960s, a heliport was built on top of the east wing of the hospital, but was short-lived.
“It was seldom used and for good reason. An adjacent elevator tower caused unpredictable air currents. When a helicopter landed, it was an event watched by many – including area residents – with some anxiety. One day, a large Coast Guard helicopter came by to try out the pad, and when it touched down, its three wheels were only about a foot from the edge of the pad.
“A management decision was quickly made that Virginia Mason should, instead, support the heliport at Harborview Hospital. Shortly thereafter, the Virginia Mason pad was quietly whisked away.”
Virginia Mason Goes Hollywood
(Excerpted from the August 1979 issue of Pulse, Virginia Mason’s employee newsletter)
“Virginia Mason Hospital got a little taste of Hollywood last month when an entourage of producers, directors, camera operators and sound engineers converged on the cafeteria and transformed it into a movie set. Among a maze of transmission wires, cameras, lights and other cinematographic paraphernalia wandered such Hollywood stars as Patty Duke Astin, Barbara Feldon, Kenneth Mars and Conchata Ferrell.
“The movie was executive producer Frank Konigsberg’s ‘Before and After,’ a film about America’s obsession with losing weight. An extensive crew from Warner Brothers in Los Angeles accompanied the producer of such TV films as ‘Pearl’ and ‘Dummy.’ Among them was Konigsberg’s assistant and location manager for the movie, Betsy Kahn. Kahn, formerly a receptionist in The Mason Clinic, was the prime force behind the decision to have ‘Before and After’ filmed in Seattle and at Virginia Mason Hospital.
“The crew and dozens of their equipment have been all over the Seattle area filming segments for the movie. Here at Virginia Mason, the filming began in the hospital cafeteria, moved across the hall to the dental offices and then outside. The final scene that concluded the movie making at Virginia Mason Hospital was filmed in room 1080 on 10 East starring a very ill Barbara Feldon.
“The scene was part of 17 days of movie making in Seattle for the cast and crew.
“‘Before and After’ is scheduled to premier on the ABC network sometime in mid-October.”
John F. Tolan, MD: Joined The Mason Clinic in 1938
(Excerpted from an interview by William Steenrod, MD, on Nov. 8, 1985)
“I went down to Ann Arbor, entered literary school at the University of Michigan and completed a combined M.S. degree in literature. Then I went into medicine in the fall of 1929 and finished medical school in 1933.
Dr. Eugene Potter’s position was associate professor of surgery. Dr. Blackford came to Ann Arbor to engage Dr. Potter and see if he would be interested in joining The Mason Clinic when Dr. Mason passed away. Dr. Blackford felt they needed somebody with a little more seniority and experience that Dr. Baker hadn’t attained at the time.
At the time, Dr. J. T. Dowling did eye, ear, nose and throat. The clinic was looking for someone to join that department. Gene called me and said, ‘Jack, this is a wonderful opportunity. You can build your own department because it’s wide open.’ I said, ‘Gene, since I was knee high to a grasshopper, I’ve been wanting to go into practice with these two brothers of mine and they have been holding a position open for me for 10 years.’ He said, ‘I know all about that. Why don’t you come out and at least take a look at it?’
Dr. Blackford and I had a very nice discussion and, just before he was about to leave the hospital, turned around and said, ‘Dr. Tolan, I wonder if you could possibly take an extra six months before coming out and do some eye work because we could use the eye help you could give Dr. J. T. Dowling.’ I said, ‘Dr. Blackford, if you’re looking for an eye, ear, nose and throat man, I’m not the person for you because six months in eye is a paltry bit of time to spend and you really couldn’t even learn to do refractions in that period of time. So, if that’s the case, I’m not interested.’
He knew that I was thinking very seriously about going to Milwaukee to join my brothers. So, Dr. Blackford said, ‘Well, it was just an idea. I thought if it were possible, and if you were interested, you might go ahead and do it.’ I said, ‘No, I wouldn’t be in the least bit interested.’ He then said, ‘Why don’t you just come out and look the place over.’
Just before Thanksgiving, we had a big snowstorm in Ann Arbor where you had to walk in the center of the road to get down to Michigan Central Depot. In Chicago, we had to get on an elevated train so we could get to the Great Northern train coming west. As luck would have it, Seattle weather was gorgeous at the time. I was here for three or four days and was very taken with the area. I then returned to Michigan and told my wife, Peg, about it.
We soon drove out west together. As soon as we got to Seattle, I visited Mr. Dare for numerous reasons, but mostly because I was broke. When I told him what my predicament was, he said, ‘This is no different from all the rest that arrived here.’
Mr. Dare put us up across the street in the Baroness. He then called the bank and told the president I would be coming down to arrange for some financial help and that he had approval from the clinic. When I joined the clinic in 1938, my starting salary was $350 a month.
Dr. J.T. Dowling lived on Bainbridge Island and had reached a point of being about 50 percent active doing nothing but eye work. He would come in about 10 a.m. and head for the ferry about 3:30 p.m. For that reason, there was a great opportunity for an ear, nose and throat man. It was a pleasure to have the chance and to build a department from the ground up.”
Nancy Lyons
Virginia Mason Seattle
“I was director of Virginia Mason’s Birth Center in the Spring of 1988 and we had just remodeled the Labor, Delivery, Recovery, Postpartum (LDRP) rooms. I received approval to purchase portable, easy-entry whirlpool tubs, which featured a side door that opened for a wheelchair transfer or for a pregnant woman to easily step into the tub. They were also appropriate from an infection-control perspective since they allowed for an antiseptic to thoroughly clean the entire system of water jets. As part of my job, I also led prenatal tours and, as a result, was very familiar with how to operate the tubs. On June 28, 1988, I was in labor at Virginia Mason with my second child. Since I had advocated for purchasing the tubs, I wanted to try them so I could tell other women what it was like to relax in them during labor. So, I got in the tub, tilted it back with the lever and filled it with water. After less than 10 minutes of enjoying the tub, I knew I had to immediately get out to have my baby. I pushed the lever forward to tilt the tub – and all of the water – forward. However, in my rush, I forgot to pull the plug and allow the water to drain, which resulted in a rush of water spilling onto the tile floor. I began yelling at my husband to clean up the mess with towels before the nurse arrived. I was so embarrassed that I hadn’t sufficiently drained the tub before tilting it forward and opening the side door. My daughter, Sally, was born minutes later! Needless to say, after resuming my prenatal tour duties, I warned other women to be sure to pull the drain plug and allow time for the water to drain before exiting the tub. Those tubs were a popular item in our LDRPs until we closed the unit in the Fall of 1996.”

Nancy Lyons
Liz Longley, RN: Impromptu Hospital Wedding Planner
(This article was originally written for Virginia Mason’s intranet, V-Net, in 2012.)
For one Virginia Mason patient, suffering a fall and ending up in the hospital was not the worst thing that could happen. The timing was the worst thing: She fell just days before her only daughter’s wedding. Suddenly an event she had dreamed of and helped plan for more than a year might go on without her.
Liz Longley, RN, Orthopedics, labored over a plan to arrange the patient’s release and transport to the wedding, but the patient declined, saying she was not about to be a distraction on her daughter’s special day. So, Longley went another way, and brought the ceremony to the patient.
First, Longley conferred with the wedding party, which secretly agreed to conduct a bedside ceremony at Virginia Mason. Next, she made sure there would be flowers and refreshments on hand. The recuperating mother of the bride had occupational therapy scheduled that day, so Longley conspired with her therapist to make getting dressed up part of her ‘therapy.’ Doing hair and make up were ‘therapeutic exercises’ as well. When the wedding party arrived, the patient found out what she was really doing – preparing to watch her daughter say, “I do.”
The bride and groom later married again, joining their guests at Seattle’s Gasworks Park. While the bride’s mother watched the second ceremony on Skype, she would always have her memory of the first ceremony, created just for her by one caring and determined nurse.

Liz Longley, RN
Virginia Mason Nurse-Midwives Provided Care to Patients at Community Clinics
(Excerpted from an article published in Virginia Mason’s employee newsletter)
“Virginia Mason remains a leader in the area of obstetrical charity care,” said Michele Domash, coordinator, Nurse-Midwifery.
“Virginia Mason has always taken seriously its responsibility to provide care for community members who have difficulty paying for medical services, and clearly demonstrates this commitment in the ties that the Nurse-Midwifery department maintains with several Seattle-area community clinics.
“The decision to devote a large portion of Virginia Mason’s charity care funds to obstetrics began in 1980, after community clinics in Seattle identified the need for better access to obstetrical services for their patients as a top priority.
“In addition, Virginia Mason felt that helping to provide a wellness-oriented, prenatal care program would be one of the best possible ways to really make a difference in community health care,” said Domash.
“Virginia Mason has ties with two local community clinic associations: Central Seattle Area Community Clinics – which links Country Doctor, International District, and Carolyn Downs Community Clinics – and Puget Sound Neighborhood Health Centers, with clinics at Columbia Health Center and High Point.
“Each community clinic serves low-income patients and uses a sliding-scale fee system.
“Three Virginia Mason nurse-midwives provide prenatal care and postpartum visits at the community clinics. They work as a team with family practice physicians from the clinics.
“These teams of practitioners then deliver their patients at Virginia Mason Medical Center, again on a sliding-scale fee basis. About 300 patients per year receive this service, which represents a substantial financial commitment from Virginia Mason.
“Larry Larson, MD, director, Obstetrics, supervises the community clinics obstetrical program, and nurse-midwives attend regular meetings at Virginia Mason to ensure that consistent standards of care are maintained throughout the clinics.
“In addition to providing direct care to community obstetrical patients, Virginia Mason – along with several other community organizations – supports a community obstetrical referral program, located at an office in the King County Medical Society headquarters. By identifying providers of low-cost and free obstetrical care in the community for area residents, the obstetrical referral program has succeeded in improving access to the health care system for many low-income women.”
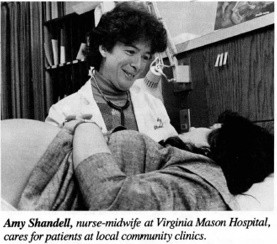
Virginia Mason Nurse-Midwives Provided Care to Patients at Community Clinics
(Excerpted from an article published in Virginia Mason’s employee newsletter)
“Virginia Mason remains a leader in the area of obstetrical charity care,” said Michele Domash, coordinator, Nurse-Midwifery.
“Virginia Mason has always taken seriously its responsibility to provide care for community members who have difficulty paying for medical services, and clearly demonstrates this commitment in the ties that the Nurse-Midwifery department maintains with several Seattle-area community clinics.
“The decision to devote a large portion of Virginia Mason’s charity care funds to obstetrics began in 1980, after community clinics in Seattle identified the need for better access to obstetrical services for their patients as a top priority.
“In addition, Virginia Mason felt that helping to provide a wellness-oriented, prenatal care program would be one of the best possible ways to really make a difference in community health care,” said Domash.
“Virginia Mason has ties with two local community clinic associations: Central Seattle Area Community Clinics – which links Country Doctor, International District, and Carolyn Downs Community Clinics – and Puget Sound Neighborhood Health Centers, with clinics at Columbia Health Center and High Point.
“Each community clinic serves low-income patients and uses a sliding-scale fee system.
“Three Virginia Mason nurse-midwives provide prenatal care and postpartum visits at the community clinics. They work as a team with family practice physicians from the clinics.
“These teams of practitioners then deliver their patients at Virginia Mason Medical Center, again on a sliding-scale fee basis. About 300 patients per year receive this service, which represents a substantial financial commitment from Virginia Mason.
“Larry Larson, MD, director, Obstetrics, supervises the community clinics obstetrical program, and nurse-midwives attend regular meetings at Virginia Mason to ensure that consistent standards of care are maintained throughout the clinics.
“In addition to providing direct care to community obstetrical patients, Virginia Mason – along with several other community organizations – supports a community obstetrical referral program, located at an office in the King County Medical Society headquarters. By identifying providers of low-cost and free obstetrical care in the community for area residents, the obstetrical referral program has succeeded in improving access to the health care system for many low-income women.”
John Walker, MD: Practiced at The Mason Clinic Starting in 1947, Chairman 1964 to 1976
(Excerpted from an interview on May 3, 1985)
“In 1933, I was in pre-med at the University of Washington. Tate Mason Jr. was a fraternity brother. I had never been in a hospital and we persuaded Tate that we would like to see some surgery.
So, on a rainy day, Tate arranged for us to come to Virginia Mason on a Saturday morning. Surgeries were probably on the 6th floor of the original building, which was the top floor. It had a skylight in it. We were cooling our heels in that little doctor’s locker room that lasted for about 25 years. We sat around for about two hours, getting rather restless waiting for Dr. Mason to let us come in and see some surgery. After a while, we were ushered into a surgery and upon a little portable platform overlooking the patient.
Dr. Mason was going to do a thyroidectomy, at which he was adept and well-known for in those days. He was one of the thyroid experts in the Northwest. And this was a time when this was an endemic area for goiters, just like Michigan. One never knows how one is going to respond to his first sight of blood. But it didn’t bother either of us at all. Dr. Mason was very gracious. I suppose Dr. Baker was there assisting him, but I didn’t know Dr. Baker. He would probably have been a resident at that point between 1933 and 1934.
Dr. Mason performed the entire surgery. It was a large goiter. I was surprised how he could get his whole hand inside the patient’s neck and down into the upper mediastinum, searching for any residue. That lasted about an hour or so and we were then ushered out.
That was my first experience with Virginia Mason.”
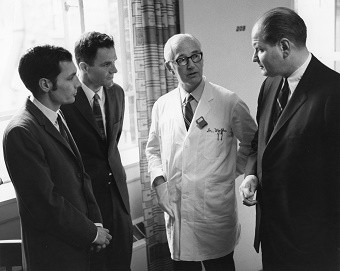
A Bit of the Unusual in the 1970s
(Excerpted from the book, “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”)
“As in previous decades, the 1970s had its fair share of unusual, and sometimes humorous, events.
“One of the more memorable happenings was known as the ‘case of the missing pigs.’ A truck load of valuable miniature pigs was being delivered at night to the research center and, in the process of transferring them, some escaped and quickly scattered throughout the First Hill neighborhood. The police department responded quickly to calls from perplexed citizens who observed some uniquely shaped animals running through their yards. All except one were ultimately accounted for. One suspects that somewhere on First Hill a barbecue was held, but this has never been confirmed.”
“Another story, also involving the research center, was that it was home to a contented seal for several months. It was being studied by scientists who were interested in hyperbaric medicine. Unfortunately, the seal was housed in a tank holding area on the roof of the research center in full view of all patient rooms on the north side of the hospital’s east wing. The actions of the seal became a topic of considerable conversation among patients, their families and the staff. Alternative housing for the seal was ultimately located.”
Kelly Richardson, RN: Outpatient Program Nurse at Bailey-Boushay House
When Kelly Richardson, RN, landed her dream job in the Outpatient Program at Bailey-Boushay House, a first priority was learning clients’ names. About 270 people access the program every week to receive drug therapy for controlling HIV, and the support services to help them stay on it. The indispensable program element is trust, so Kelly started by walking the halls, greeting clients by name. Some looked surprised.
“Sometimes they’d thank me for knowing who they are,” said Richardson. “I think it’s a population that’s really misunderstood. They all have a story. It’s unbelievable what they’ve been through and survived.”
HIV medicines not taken consistently can cause viral resistance, and that resistance can be transferred to others. Bailey-Boushay’s Outpatient Program fills a critical role by providing and monitoring complex medication regimens to prevent AIDS and the spread of HIV in the community. Along with medication, clients can get a meal, shower, access counseling and basic health care, use a computer, join group activities or simply socialize with others.
For Richardson, every client visit is a chance to build a relationship: a key determiner of success with medication adherence. If a client comes in and needs to talk, her nursing colleagues can cover the floor, giving Richardson the gift of time with a client.
"My favorite part of the job is listening and engaging with our clients," said Richardson. "When they open up to you, it’s the best feeling in the world."

Teresa DeMarce
Virginia Mason Seattle
“I was born at Seattle’s Doctors Hospital in 1957. Since I had never heard of it, I researched the history of Doctor’s Hospital and learned that Virginia Mason was literally attached to it many years ago. So, when I went to First Hill recently, I located where that part of Virginia Mason was attached to Doctor’s Hospital way back when. Congratulations on your centennial, Virginia Mason!”
Caroline Kratz
Virginia Mason Seattle
"My mom and dad met at Virginia Mason in 1981. She was a pharmacy technician and he was an engineer helping to install the new intravenous therapy room. They went on some of their first dates in the hospital cafeteria. One thing led to another and, in 1983, my parents got married. As my dad continued to work at Virginia Mason, our family began to grow until there were four of us. I am the youngest. Every December, just before Christmas, we would come pick my dad up in the turnaround off of Seneca Street so we could take our Santa picture downtown. As we waited, I can remember thinking that my dad worked at the best hospital in the city! It was pure magic coming downtown around that time of year with all the lights and decor around Seattle and the hospital. I recall watching doctors, nurses and patients walk across the sky bridge and wondered if I would be there someday, treating patients in the heart of the city. In 2005, my older brother Larry Jr. joined Virginia Mason as a patient transporter and eventually worked his way into the Engineering department. In 2006, my other brother, Chris, began volunteering in the hospital during high school, and in 2018, he was hired as a perioperative equipment technician. In 2015, I joined the Sports Medicine Department as a physical therapy aide. Since then, I was recently accepted into physical therapy assistant school and have begun pursuing the next big step in my career, Feb. 14, 2020 was the last day that my dad, my brothers and I worked together at the hospital. Virginia Mason has always been a place that is truly like home for our family and it holds a big place in each one of our hearts!"

David Wilma
“In 1974, I was a federal narcotics agent and rolled my car while pursuing smugglers near the Canadian border. I landed upside down at the bottom of a ravine, where a member of the Royal Canadian Mounted Police found me and pulled me out through a window. I had broken ribs and a collapsed lung.
“Once I was released from intensive care in Bellingham, I went for a follow-up visit with the The Mason Clinic doctor who performed our executive physicals. I figured the clinic could just bill the government and keep the cost out of my own health plan. He was also the only physician I had seen in years. The doctor promptly ushered me to a radiologist nearby. The films revealed that the damaged lung was filling with fluid and the pericardium – the membrane around my heart – was filled with blood. He immediately admitted me to Virginia Mason Hospital.
“As a young, fit specimen with a traumatic injury, I was of great interest to the interns and resident. I was the only patient on the floor under the age of 60 not suffering from emphysema. Each physician took my history and examined me, which got tiresome after a while. An intern removed the fluid in my lung with a long needle in my back, while a veteran nurse comforted me. The intern then proudly showed me a glass container filled with red fluid. After other tests, like a bronchoscopy – where I was administered cocaine in my nose – I was advised that my life-endangering issues were resolved. Life endangering? I guess Virginia Mason saved my life.”
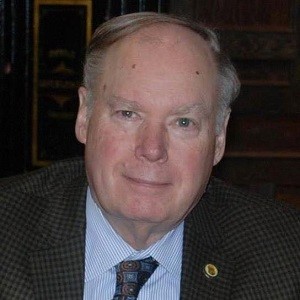
David Wilma
Thomas Carlile, MD: Virginia Mason Physician (1939-1974)
(Excerpted from an interview by William Steenrod Jr., MD, on May 25, 1988)
“In 1936, my parents and I drove from Ann Arbor to Washington for a visit with an aunt and uncle. We spent two weeks in Seattle and I was very impressed with the city. The sun was out for the two solid weeks in June and Mount Rainier was beautiful. I decided it was one of the places I would like to live. About that time, I read about the death of Dr. Mason Sr. and was impressed with the drama of a man being installed American Medical Association president on his death bed at Virginia Mason Hospital. I was a sophomore at the time.
In 1938, I applied to Virginia Mason Hospital as an intern and, to my surprise, was accepted because I was told they did not accept married interns. I was so gung ho that I arrived in Seattle early. It was July 25, 1939. I wandered around the hospital and met several people, including one of the interns who was departing. He immediately proposed that I start work the next day, so he could leave early. I was so anxious to get going, that I took him up on it.
At that time, there were four interns and two residents. I was on a rotation called First Medicine, which was a hospital service. I began the life of an intern in those days earning $25 a month. I put in the pretty characteristic days as an intern, one night on and one night off, working all day on Saturday and every other Sunday off.
This was the first year they accepted married interns. So, Bob Williams*, George Hollenbeck and our wives rented a very luxurious apartment at 16th and Madison for $100 a month. It had four bedrooms and four bathrooms. My wife made $75 per month as a secretary in the clinic, plus $10 each month for doing all the hospital operator reports.”
(* Dr. Robert Williams was killed in action serving in the U.S. Navy in 1942.)
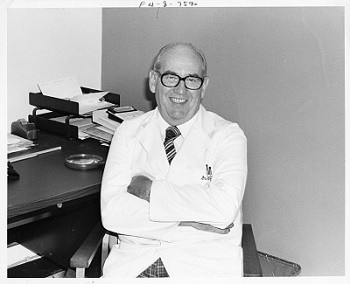
Thomas Carlile, MD: Virginia Mason Physician (1939-1974)
(Excerpted from an interview by William Steenrod Jr., MD, on May 25, 1988)
“In 1936, my parents and I drove from Ann Arbor to Washington for a visit with an aunt and uncle. We spent two weeks in Seattle and I was very impressed with the city. The sun was out for the two solid weeks in June and Mount Rainier was beautiful. I decided it was one of the places I would like to live. About that time, I read about the death of Dr. Mason Sr. and was impressed with the drama of a man being installed American Medical Association president on his death bed at Virginia Mason Hospital. I was a sophomore at the time.
In 1938, I applied to Virginia Mason Hospital as an intern and, to my surprise, was accepted because I was told they did not accept married interns. I was so gung ho that I arrived in Seattle early. It was July 25, 1939. I wandered around the hospital and met several people, including one of the interns who was departing. He immediately proposed that I start work the next day, so he could leave early. I was so anxious to get going, that I took him up on it.
At that time, there were four interns and two residents. I was on a rotation called First Medicine, which was a hospital service. I began the life of an intern in those days earning $25 a month. I put in the pretty characteristic days as an intern, one night on and one night off, working all day on Saturday and every other Sunday off.
This was the first year they accepted married interns. So, Bob Williams*, George Hollenbeck and our wives rented a very luxurious apartment at 16th and Madison for $100 a month. It had four bedrooms and four bathrooms. My wife made $75 per month as a secretary in the clinic, plus $10 each month for doing all the hospital operator reports.”
(* Dr. Robert Williams was killed in action serving in the U.S. Navy in 1942.)
Contract medicine
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
As the Mason Clinic and Virginia Mason Hospital began its second decade of existence, it appeared to be a thriving health care organization in Seattle. But those early days of prosperity soon began to evaporate as the Great Depression swept throughout the country. The clinic doctors met this crisis with an innovation that made economic sense. Since the beginning of their practice, the clinic doctors had contracted to provide medical care to the employees of various organizations. Now, they began seeking out more prepaid medical contracts with large corporations. As a result, contacts were written with the Boeing Airplane Company, American Mail Lines, Rhodes Department Store, Frederick & Nelson, the US Post Office and the Seattle Police Department. This was one of the earliest prepaid medical plans in the Pacific Northwest. The contracts were finally transferred to the King County Medical Service Corporation when its Medical Service Bureau was founded in 1934, which were King County Medical’s first contracts.
Virginia Mason’s 1,000th Living Donor Kidney Transplant
On Aug. 6, 2019, Virginia Mason performed its 1,000th living donor kidney transplant. This was significant since less than 15 percent of the 314 transplant centers in the United States had accomplished this. The Virginia Mason Transplant Center, which opened in 1972, was the first kidney transplant program in Washington state to reach this milestone.
The achievement was testament to medical and surgical advances in organ transplantation, which have led to successful outcomes for kidney transplant recipients. The success of living kidney donation has created a life-saving option for waitlisted kidney transplant recipients who often wait years for a deceased donor kidney. Virginia Mason’s focus on safety and optimizing the patient experience has contributed to the great success of its living donor program.
“To spare patients in need of kidneys long and uncertain wait time on the transplant list, it’s more important than ever for relatives, loved ones, friends and even individuals who wish to remain anonymous to serve as living donors,” said Andrew Weiss, MD, nephrologist and medical director, Virginia Mason Transplant Center. “In fact, nearly 7,000 transplants nationwide were made possible in 2018 by living donors.”
The 1,000th living donor kidney transplant at Virginia Mason involved a married couple, Daniel (Dan) and Kelli Campbell, from Pullman, Wash., who met while students at Eastern Washington University in Cheney, Wash. Dan donated a kidney to Kellie, who had known for much of her life that she might need the life-giving procedure due to an autoimmune disorder that caused her kidney disease. Kelli received confirmation just nine months earlier that she needed a new kidney.
Although Dan knew he wanted to try and donate one of his kidneys to Kelli about 20 years ago when he learned about her condition, the father of two and Washington State University administrator found out about a month before the transplant that he was a match.
“There are thousands of people waiting for a kidney transplant where live donation is their best option for a long, healthy life. Live donors go on to live long, active lives,” said Dan. “If more people explored the option of donation, we could make each others’ lives and our communities stronger.”
The kidney disease Kelli has causes fatigue, dietary changes and limits on some common over-the-counter medications. It has also made some life experiences, like pregnancy, dangerous.
“We are grateful that Virginia Mason is doing such great work, but there are many other people waiting,” said Kelli, who works at the Whitman County Courthouse in Colfax, Wash. “However, the fact that this is the health system’s 1,000th living donor kidney transplant speaks to the quality of the program, their outcomes and how great the need is.”
When asked what she was looking forward to most after recovering from her kidney transplant, Kelli said, “I’m looking forward to seeing our children become adults. And in the meantime, I want to return to an active lifestyle, ride bikes with my family and eventually travel.”

Left to right: Donor surgeon Nick G. Cowan, MD, Urology; kidney recipient Kelli Campbell; kidney donor Daniel (Dan) Campbell; living donor advocate Jessica Spiers, LICSW; and Virginia Mason Transplant Center Medical Director Andrew Weiss, MD, Nephrology.
Victoria Gempesaw
Virginia Mason Seattle
“I was born at Virginia Mason almost 25 years ago and it’s also where my parents met. I have seen how much of an impact my mom makes here on a day-to-day basis, so I started to volunteer here at the age of 18. It was shortly after when I continued my service as a volunteer in Administration, then on Jones 18, and now the Outpatient Infusion Center. As a pre-nursing student who hopes to become an RN one day, I am employed as a patient care technician (PCT) in Med-Surg and have had a miraculous experience with the nurses, PCTs, staff and patients here. It has been a huge transition, but the leadership here has been so amazing with their support and guidance. I truly believe that Virginia Mason is one of the top hospitals here in Seattle and I’m so proud to be part of it!”
Tracey Croisier
Virginia Mason Seattle
“In March 2017, I had a heart attack and was diagnosed with a rare congenital heart blockage. The doctor that found the blockage insisted the blockage was not causing my chest pain. So, I ended up flying to Stanford for a new surgery to fix the problem. I clearly needed a new cardiologist and luckily found Dr. Drew Baldwin. I have had several post-op complications and Dr. Baldwin has attentively tended to me with compassion and thoroughness. Also, David Cowan in Cardiac Rehab was instrumental in getting me back to exercising without fear. I had the odd luck of visiting five hospitals in 12 months. Virginia Mason and Stanford are head and shoulders above the rest. In addition to great bedside service and medical professionals that take heart problems seriously, Dr. Baldwin said he was happy to refer another patient to the surgeon at Stanford. He had also thought congenital heart blockages were only treatable with medication and said he was so impressed with how Stanford healed my blockage that he was glad he could refer out. How often do doctors thank patients? Almost never.”
James Simmons, MD: Practiced at Virginia Mason Starting in 1974
(Excerpted from an interview by John Kirkpatrick, MD, on Sept. 3, 2015)
“The federal government helped bring me to Virginia Mason. I had a draft deferment with the Public Health Service and wanted to serve in a clinical setting, rather than with the National Institutes of Health or in a township, etc. So, I was sent to the old Marine Hospital, which was fortunate because I loved Seattle and the Northwest.
“I got a lot of experience in ambulatory medicine there, which I’d never had during my training program. I learned a lot from the physician assistants about how to take care of adults in outpatient settings.
“In 1972, with support from Chairman Dr. Joel Baker, the partners decided to form a section of General Internal Medicine. We thought we should get some primary care doctors – internists or emergency medicine physicians. It was decided that if we wanted to keep our specialists busy, we needed to have generalists taking care of people locally so they could refer to the specialists. We were warmly welcomed by many of the sub-specialists.
“When I first came to the clinic, I saw a lot of Alaskans. When they came to Seattle, they would see a number of sub-specialists based on their condition. Many were disappointed because I didn’t send them to a bunch of specialists. I didn’t think they needed it.”
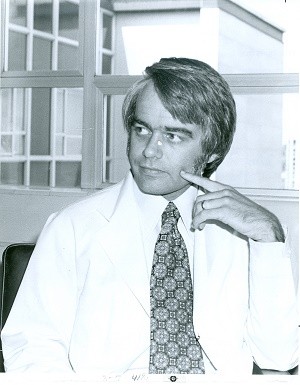
Ties to Alaska
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
During the Great Depression years, various factors helped the Mason Clinic’s reputation grow as a specialty group practice and diagnostic center. For example, many companies that were sending employees to Alaska arranged for thorough diagnostic workups at Virginia Mason. Through the years, strong ties between Virginia Mason Hospital and small communities in The Last Frontier developed, many of which remain today. These relationships were furthered by the fact that numerous physicians who trained at Virginia Mason ultimately went to Alaska to practice, which resulted in many referring complicated cases to the hospital and clinic doctors.
Joel Baker, MD: Surgeon (1929-1970), Chief of Surgery, Chairman 1945-1964
(Excerpted from an interview by William Steenrod Jr., MD, on May 14, 1986)
“I grew up in a small town of about 1,800 people in Shenandoah, Virginia. My uncle, who lived there, was a physician to the town. This was in the horse-and-buggy days and the livery stable kept two teams ready for him to go at all times. I would often skip school to go with him, and he never told my mother.
I went with him all over the Blue Ridge Mountains of Virginia in horse and buggy. In the winter, we went in a sleigh with the horses and a robe to cover us up. He would thaw my hands when they got cold and ride along in the mountains singing ‘Oh, dem golden slippers!’ As I grew up, I never thought of being anything but a doctor. I always wanted to be a general practitioner in a small town. That was my ideal.
I went to the University of Virginia Medical School and graduated in 1928. In my last year, I met Dr. Tate Mason and he spoke with me about coming to Seattle.
Dean Flippen thought I should go to St. Luke’s in New York. I said I’d rather go West. So, I came by train, which was a three-day trip in 1928. I still have the original telegram and letter of contract from Mr. Lewis A. Dare. It paid me $50 a month, which was pretty good wages then. It also included my train fare both ways. But, I never used the return fare. I talked two classmates into joining me, Louis Edmunds and John Wilkerson.
Dr. Mason often told me about his contacts with his patients in the coal mines and how it molded his judgment in seeing the patient’s family problems as well as their illnesses. I think maybe that was the reason he thought it was a good thing to take house calls, which he did.
One day, I was called down to what is now Denny Regrade (Belltown) to see a sick young man. He was about 20, lying there sick in an apartment. His mother was drinking beer as I was examining him. It was obvious he had an acute appendicitis with all the classic signs and symptoms. I said, ‘We have to take you to the hospital to have an operation. Dr. Mason will have to take your appendix out.’ About that time, the mother who hadn’t spoken, said, ‘You will not do any such thing. You are just a kid. I want to get a responsible doctor here to see him. Although I did look very young then, I replied, ‘Ma’m, that’s fine, it’s your son that has the appendicitis, not I. I feel fine. Thank you very much. I’ll bid you a good day.’ I started for the door and the son said, ‘No, no, you come back here.’ Then the mother changed her tune and said, ‘No. Doctor. I didn’t mean that.’ They did exactly as I said after that.”
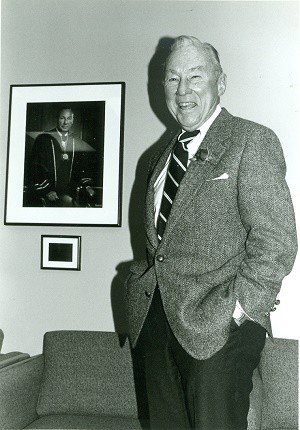
Ties to Alaska
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
During the Great Depression years, various factors helped the Mason Clinic’s reputation grow as a specialty group practice and diagnostic center. For example, many companies that were sending employees to Alaska arranged for thorough diagnostic workups at Virginia Mason. Through the years, strong ties between Virginia Mason Hospital and small communities in The Last Frontier developed, many of which remain today. These relationships were furthered by the fact that numerous physicians who trained at Virginia Mason ultimately went to Alaska to practice, which resulted in many referring complicated cases to the hospital and clinic doctors.
Tina Boyd
Virginia Mason Seattle
“I had my son Victor at Virginia Mason 34 years ago in 1985. I still remember the fancy dinner that was served to parents afterwards. It was steak and lobster! I love to tell that story, even today. I have wonderful memories of the birth of my child. The staff at Virginia Mason were always polite and friendly. They would bring my baby in for a feeding and then take him back to the nursery so I could sleep. I hear things are much different today. A year ago, I happened to walk through the unit and pass by where the nursery use to be. It almost brought me to tears. I could not have chosen a better place to have my one and only son.”
Virginia Mason Urology Team Members Traveled to Africa for Mission Work
(Excerpted from a Health & Wellness blog post written by Una Lee, MD, FPMRS, Urology)
“It was my third trip to Mbarara, a bustling city in rural Southwest Uganda and home to a regional hospital. I felt excitement but also a new responsibility: this time I would serve as trip medical director of Medicine for Humanity, a nonprofit organization dedicated to improving women’s health, in partnership with the Mbarara University of Science and Technology. The mission had grown, but it felt like a homecoming – a connection I needed more than I knew.
“The visiting team included three Virginia Mason colleagues: Brooke Reagan, surgical technician; anesthesiologist Carli Hoaglan, MD, and urology fellow Wai Lee, MD. We and our volunteer counterparts became a well-oiled machine from the moment we met, organizing 22 bagged loads of medical supplies and gear.
“The Virginia Mason team moved into a university-provided house, and soon we would familiarize ourselves with the local food, sights, smells, as well as traditions like mid-morning tea with chapatti and samosas. We would also come to know operating rooms stripped to the basics. Sometimes the power would go out and we would keep operating with flashlights and cell phones to illuminate the surgical area.
“Our mission was two-fold: to collaborate with and teach Ugandan surgeons, and to provide fistula surgery to the region’s women in need. It is a sad but common story that many young Ugandan women suffer traumatic childbirth. Surgical repair is the only way to restore function and enable these women to return to their lives and communities.
“Radio announcements were made of our medical team’s arrival, bringing local women by way of compact ‘boda boda’ motorcycles, busses and on foot from area villages. Every member of our surgery, anesthesia and operating room teams worked with a common purpose and a joyful attitude, helping us accomplish so much with so little. It was invigorating to work with such an amazing team of people – American and Ugandan – from sunrise to late into the night.
“During the two-week mission, our team focused on doctoring, operating and teaching, without the barrage of other pressures and demands that would normally fill our workdays. We arrived in Uganda to offer surgical care and education, but through the process of talking, laughing, sweating, celebrating life and grieving loss together, we realized the Ugandan people were giving us more than we could ever give in return. With each smile, hand held, or moment of recognition of our shared human experience, we were restored.
“My time in Uganda changed me. I felt the true joy of being a doctor and a teacher. I was humbled by the privilege of helping these women on their path to healing. And now, back in my regular life as a physician in Seattle, I am approaching each patient with the joy and openness that I learned from the Ugandan people.”

Dr. Lee teaching Ugandan and American residents and fellows.
Randi Anderson
Virginia Mason Federal Way, Virginia Mason Kirkland and Virginia Mason Seattle
“Although I was not born at Virginia Mason (my husband was, though!), all of my pediatric care was at Virginia Mason Kirkland. So, for as far back as I can remember, Virginia Mason was synonymous with my health and wellbeing. My whole family had all of their care at Virginia Mason. So, naturally, when I was a teenager and needed shoulder surgery, we sought care there. I did all my shoulder rehab at Virginia Mason, which was such an awesome experience that I decided it’s what I needed to do as a career. I went off to college but returned to Virginia Mason to complete a 400-hour, unpaid internship for my bachelor’s degree. After graduating, I called the clinic where I had completed my internship (Sports Medicine), asked for a job and was hired! That was in 2004. Since then, I have worked in Sports Medicine, the Kaizen Promotion Office, in leadership at the Federal Way and Seattle clinics, and now in leadership at the Jones Learning Center. Since my kids receive all their care at Virginia Mason, the story will start anew!”
Virginia Mason School of Nursing
(Excerpted from the book, “Vision and Vigilance: The First 75 years, Virginia Mason Medical Center, 1920-1995”)
Between 1925 and 1952, 579 nursing students graduated from the hospital’s nursing school. In 1957, the school was assimilated by the University of Washington’s program as it became difficult for Virginia Mason to finance the nursing education program. “Probies,” as the entering students were called, lived in an old house on Spring Street. The students lived on the first two floors. There were two bathrooms shared by all. Students were not allowed to address each other by first names while on duty and the hours of study and work were long. It wasn’t until 1946 that the new nursing school residency hall – named Blackford Hall – was completed, which was an event welcomed by all. (In 1956, Blackford Hall was converted to the Research center.) In 1940, nursing students began wearing a plain white uniform. Nursing caps were mandatory and fines were levied if students showed up without one. Discipline was intense in other areas as well. Students were required to stand whenever a physician or senior nurse entered the room. Pay was $10 per month, which increased slightly to $15 per month during World War II. The capping ceremony took place after three to six months and was a very formal affair, which was often held at the Women’s University Club. At graduation, Dr. Mason or a member of his family would present a red rose to each student – a tradition that meant much to all.

Virginia Mason Nurses, Class of 1928
A Commitment to Aesthetic Improvement
When the hospital addition was under construction between 1973 and 1974, Virginia Mason invited members of a Renton arts club to paint scenes on the barrier wall.
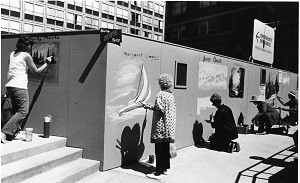
Penny Zefkeles
Virginia Mason
“Every Virginia Mason location and doctor has provided me with the best care – from Dr. Teng, who made house calls; to primary care from Dr. Trigg, who learned all my health and personal matters; and now with Drs. Kita and Peng helping me with my recently diagnosed multiple sclerosis. I feel very lucky to have been cared for by them all. Virginia Mason is a great medical center. I feel blessed!”
Patrick Mahoney, MD: Practiced Pediatrics at Virginia Mason Starting in 1968
(Excerpted from an interview by John Kirkpatrick, MD, on Oct. 5, 2015)
“Dr. F. Richard Dion and I had kind of a hard start to begin with because Boeing tanked and after we teamed up, we weren’t too busy. But we were lucky to be a part-time practice. Fortunately, as time went on, it thrived.
“The Mason Clinic is a wonderful place to practice. There are several things that make it unique. One is the fact that we were partners and had a small percentage of The Mason Clinic properties as part of the partnership. That meant we owned the business and really needed to go the extra mile. Sometimes that meant working later than normal. We were all trying to make it an exceptionally effective place and it was. Another thing was that in the ’60s, the National Institutes of Health produced a large number of specialists and there was a big pool to search from. I think the very best people could come to The Mason Clinic.
“Colloquia is a term Dr. Ed Morgan came up with. It’s where a group will leave their workplace and go somewhere else to discuss how to make things better. That was good … a way of really integrating with all the specialists. It paid off. You knew people well enough that if you asked them to do something, they’d be very happy to do it.
“I also think the sabbatical was a good idea. It may be controversial, but it was really important, in my case, because I used the opportunity to be a guest editor for Pediatric Clinics of North America. That work helped establish us as a center of endocrine specialty. It was an example of the many ways that The Mason Clinic helped.”
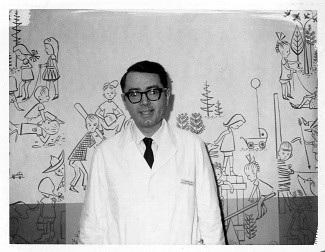
Patrick Mahoney, MD
Dennis O'Loane
Virginia Mason Kirkland
“I have been a patient at Virginia Mason Kirkland Medical Center since it opened. I was blessed to have been assigned to Dr. Kaplan as my physician. My care has always been exceptional, not only by the staff but thanks to Dr. Kaplan, as well. Virginia Mason also saved my life with outstanding cardiac care after a heart attack. I have been called an advocate for Virginia Mason during this time. I am very proud to be a Virginia Mason patient.”
Fred Cleveland, MD: Elected Mason Clinic Chairman in 1976
(Excerpted from the book, “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1975)
“Fred Cleveland, MD, a cardiologist, was elected Virginia Mason chairman in 1976 and served one term. Because of a partnership-mandated age restriction, he was not eligible for an additional term.
“Dr. Cleveland brought a slightly different leadership style to the group. For example, he placed little value on what he viewed as organizational work that, in his opinion, didn’t need to be done. He elected to break with the tradition started by previous chairmen of preparing a comprehensive, annual written report for clinic partners.
“An avid fisherman and wine connoisseur, Dr. Cleveland projected an image of self-sufficiency that he expected others to understand and accept. Independent, yet supportive of the group, he led the organization during a transitional period when the partners debated issues of growth with increasing intensity.
“Like his predecessors, Dr. Cleveland did not have any problem with decision-making. He expressed opinions that he had carefully reasoned out and made pronouncements with a dramatic flair. But he also had the ability to change a course of direction if convinced that it would be in the best interests of the group or individual.
“One of his strengths, appreciated by physicians and administrators alike – and common to all of the elected chairmen of the group – was his sense of fairness.
“Bob Riggens, MD, remembered Dr. Cleveland this way: ‘First and foremost, he was always forthright and honest. If you asked him a question, and he didn’t know the answer, he’d say so. If he gave you an answer, it was what he believed to be true, and he’d always stand behind his statement or commitment. He was a gentleman and had a strong sense of integrity. He didn’t partake in gossip, especially if the conversation was derogatory to a colleague or the organization, of which he was very proud. His patients loved and respected him, feeling that he was always their advocate. When he was our section chief, and later as chairman, we felt the same respect and allegiance.”
“People respected his ability to remain calm when something wasn’t going right. He expected performance but was absolutely forgiving. Under his supposed gruff style, Dr. Cleveland was a gentle person and it was a great loss to the organization when he died of cancer in 1989.”

Fred Cleveland, MD
Chris Stewart
Virginia Mason Seattle
“Virginia Mason has always been synonymous with family for me. Currently, there have been three generations of Stewarts that have worked, or are, working here. My mother-in-law, Diane Stewart, worked at Virginia Mason in the 70s as a Radiology Technician and head of Special Procedures under Dr. Burnett. When I moved to Seattle and was thinking about getting into health care, she mentioned Virginia Mason and lo and behold I ended up here more than 18 years ago. I could not imagine working anywhere else! My oldest daughter, Erin Stewart, recently graduated from college and asked for guidance on what to do next. I immediately referred her to Virginia Mason. She is currently working in the Insurance Billing and Follow-Up department and is loving it. She especially likes to attend Friday Report Outs and Virginia Mason Production System (VMPS) collaboratives to learn more about the ‘VMPS’ thing I have been talking about for the last many years.”
Bridget Frederick
Virginia Mason Seattle
“I was diagnosed with polycystic kidney disease when I was newly married 25 years ago. Never in a million years would I have thought I’d need a kidney transplant, but my husband said it was that moment he knew he would be the one. In 2013, the unthinkable happened. My kidneys were failing fast and I was placed on dialysis and the transplant list. Several family members jumped in the donor program, but it was my husband, Rob, who – in the end – became my donor and saved my life. We were only the second transplant in Virginia Mason’s history, so we were told, to participate in both a donor and recipient no-blood transplant. It has been almost six years and we are both doing great and back to doing all the things we love while enjoying life. This is all thanks to the support of our family and the care, concern and dedication to details of my nephrologist, Dr. Thompson, and our transplant team: Drs. Kuhr and Kozlowski and the Transplant Center team.”
Bethany Suhn
Virginia Mason Seattle
“My entire nursing career has been here at Virginia Mason. From my very first clinical in nursing school, to my current role as assistant nurse manager, and all in Oncology. Fifteen years and counting. I can’t think of a better place to be!”
First Hospital to Use IV Injection of Sodium Amytal for General Anesthesia
On June 15, 1929, Virginia Mason became the first hospital in the United States to use intravenous injection of sodium amytal for general anesthesia during a thyroidectomy operation.
Virginia Mason Hospital made a film about it at the time. University of Virginia Medical School graduate Joel Baker, MD, was present for the surgery.
In 1998, he said, “I had just become assistant to Dr. Mason … out of internship. We had the anesthetist monitor the patient, but I gave the intravenous sodium amytal for Dr. Mason to do the thyroidectomy. We had a number of guest doctors watching. I have a picture of it at home. The patient slept over a day and I didn’t sleep any during that time. When she awakened, she was perfectly normal, didn’t remember anything about it and was in excellent shape. It was a nervous time for me.”
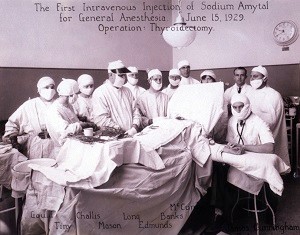
Virginia Mason Team Member Recognizes Photo of Her Uncle in Centennial Video
(Submitted by Ede Cooper, quality assurance and safety manager, General Lab)
“While watching the video, ‘Virginia Mason: A Century of Innovation,’ my eyes widened at the 3:25-3:27 minute mark when I spotted a picture of my uncle, Carl. He played a critical role in helping install Virginia Mason’s hyperbaric chamber.
“In the picture, he is wearing a headset and clean-shaven beard. I recognized him immediately because of the headset since, in his spare time, he was a private floatplane pilot who let me fly his plane with him.
“Carl married my father’s younger, and only, sister before serving in the Navy during the Vietnam War. His skills working on diesel submarines with sonar were among his many wonderful, innovative attributes.
“He was also a hard hat diver and I’ve seen pictures of him in his gear. His knowledge and skills below the water creates an image of his adventures like in the novel, ‘Twenty Thousand Leagues Under the Sea.’
“After learning more about our Virginia Mason Medical Center connections earlier this year, I shared the centennial video with him. Since it was many years ago and the photo’s shadowing inhibits clarity, Carl was not sure whether it’s him in the hyperbaric chamber at the 3:18-3:19 minute mark or the guy standing to the right.
“Regardless, I was excited to see his contributions help make history even more special for me and Virginia Mason.
“My family and I count on the medical center for our health care and regularly recommend the health system to friends.
“Happy 100th anniversary, Virginia Mason!”
Sara Abernathy
Virginia Mason Federal Way and Virginia Mason Seattle
“I am a type 2 diabetic and end-stage renal failure patient. I am blind in my left eye and on dialysis. All of this means that I’m hospitalized a lot. Everyone at Virginia Mason – from patient care technicians to physicians – are a huge part of my life. Virginia Mason is my second home. They are learning much from me. I hope my life and story are part of why Virginia Mason will be around in another 100 years collecting more stories of the lives they impact. I would like to use my life to change others’. If my life story can positively affect just one person, it’s worth it. I am passionate about helping people live their best life. Thank you for keeping me alive!”
ICU patient inspires health care team
(Excerpted from Virginia Mason’s November 1989 Pulse newsletter)
“Incredible.” That’s how nurses in ICU describe 36-year-old patient Margie Clement, who spent five months on their unit. Clement was brought in May 6 with botulism, which caused total paralysis. As a result, Clement spent several months on a ventilator, receiving intravenous feedings. According to her nurses, it was Margie’s inner trust, strength and determination – as well as the support of her family – that enabled her to survive. The story has a happy ending. Clement finally left the ICU on Oct. 18, spent a short period of time in rehab, then returned home to her husband, Gary, and their three children in Sequim, Wash. Soon, she will resume all her former activities. On the day Clement left the ICU, her physicians – Drs. John Ravits and Richard Winterbauer – threw a party for Clement and the entire health care team that cared for her. Both physicians thanked everyone for pulling together so magnificently in caring for Clement. Claire Fisher, RN, summed up the feelings of many who had gotten to know Clement well. “For all the nurses, to see this person struggling and winning gave us all hope. She was just incredible.” Fisher, Susan Vitaljic, Melinda Eitscheid, Roxanne Tervola and Melanie VanderWeerd were primary nurses for Clemens.
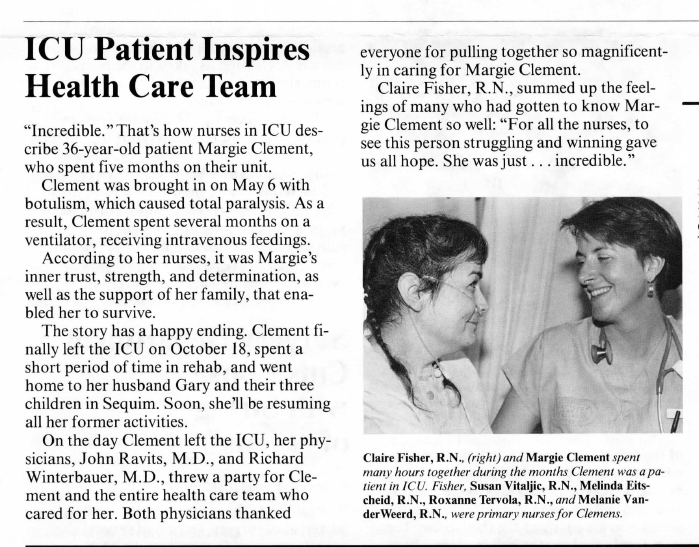
Milton Katims: Seattle Symphony Conductor for 25 Years
(Excerpted from an interview circa 1994)
“I arrived here in 1953 to guest conduct the Seattle Symphony. I was here as conductor from 1954 to 1976 and then another three years as principal guest conductor.
“There is something very wonderful about conducting an orchestra in this size city rather than in New York. After a concert, I’ll go to a supermarket or to the cleaners and someone might say, ‘I was at the concert last night and I heard this or that.’ The funniest experience I had was, after a concert one night, my wife, Virginia, said, ‘You have to put the garbage out.’ So, in my white tie and tails, I rolled the can out to the sidewalk as a car drove up across the street. Although I couldn’t see inside, someone inside the vehicle said, ‘Oh, the Beethoven tonight was beautiful, maestro.’
“I started at the clinic sometime in the early ´60s. I liked my appointments very much. I’ve always felt there’s a tremendous affinity between medicine and music.
“My personal physician was Dr. Fritz Fenster until he decided to give up practicing and go into administration. That was a big mistake, in my opinion, because I thought he was one of the best gastroenterologists in the country.
“Despite what else may happen to me, I just want to be able to keep playing tennis.”
F. Richard Dion, MD: Practiced at Virginia Mason Starting in 1962
(Excerpted from an interview by John Kirkpatrick, MD, on Oct. 5, 2015)
“After graduating medical school from the University of Minnesota in 1955, I practiced pediatrics for seven months then got drafted into the Army. They sent me to practice by myself in a remote part of Turkey. It was an interesting experience. I was glad to get back to Mayo Clinic. I had a friend, Dr. Pat Ragen, who was with The Mason Clinic at the time. He informed me they were looking for a pediatrician.
“This seemed like something I might be interested in … a group of practitioners, something like the Mayo Clinic, in a part of the country I liked. There was a series of communications with the personnel committee, headed by Dr. Luke Hill. Eventually, Dr. Bill Crenshaw came to Mayo and interviewed me. I came to Seattle, was royally entertained by the group and started in January 1962. I practiced here by myself until 1968, when Dr. Pat Mahoney joined me and I was glad to have him.
“I was doctor No. 40. It was a partnership. New people entered as associates and you were an associate for three or four years before you may or may not be admitted to partnership. Partnership meant you were accepted as one of the group and ponied up money to become a partner at a certain percentage. Depending on your percentage, it cost you various amounts of money, which they were happy to lend you at a reasonable interest rate. That’s the way it worked in those days, until the partnership was abandoned and it became a non-profit entity.
Having been at Mayo Clinic, I appreciated being part of a multi-specialty group who were practicing at a high level.”

Marilyn McQuillan, RN, and F. Richard Dion, MD. Dr. Dion is holding the first pair of twins to be patients of the Pediatrics section of the Mason Clinic
Charles Karr
Virginia Mason Seattle
“I was born in the Virginia Mason Hospital in downtown Seattle on Oct. 8, 1929, which was nine years after it opened. All three of my sons were also born there, between 27-33 years later. I still use Virginia Mason Health System for all my medical needs and I'm now 90 years old. Congratulations to all of the many caregivers who have served us well over so many years.”
Janet Walthew
(Excerpted from an interview with David Wilma on Jan. 28, 2019)
“I came to work at Virginia Mason in 1972, when my husband was in his last year at the University of Washington. We had two small children and I saw an ad in the paper for a part-time cashier. It paid $2.53 per hour. I thought I’d stay here until I graduated and ended up staying 25 years. One day, somebody called in sick and they asked me to answer the phones. Since my dad had been a bail bondsman in the Tri-Cities, I knew how to collect money. One thing led to another and I ended up managing Patient Accounts.
“I knew how to speak with people and help them find a solution to how they could pay their bills. We also charity care, but it wasn’t formal with applications. Since we had received money from the Hill-Burton federal program after the war, we had an obligation to give uncompensated care and report it annually.
“We would look at every patient that was admitted every day and verify their insurance. We would find out what kind of health plan they had through a form we would send to the insurance company. There was no internet and we rarely made a long-distance phone call because of the expense.
“Medicaid was very difficult to secure funding for patients because they could not have more than $2,000 in assets, including the value of their car. We had a courier that went down to the Medicaid office every day and took our applications. Patients could get on Medicare as soon as they had a kidney transplant or after so many months on dialysis. That was a whole new funding source for patients.
“If we had an uninsured patient and couldn’t get them funded for Medicaid, I would go across the hall to the Medical Education office and summarize the patient’s scenario to the head of Medical Education, which was Dr. Robert Heckstrom followed by Dr. Jim Coatsworth. They would look into the case medically to see if it might be a good learning opportunity for residents. I don’t think I ever got turned down. They would put a resident in charge of the case and attending Virginia Mason physicians that would oversee everything. The patient would not receive a professional charge from the Mason Clinic and the hospital bill was on a sliding scale … from zero to a percent of the bill. A lot of times they were surgical cases.
“I organized charity care to raise funds for uncompensated care. One year, we had a little boy who was deaf and an orphan. He received a cochlear implant from Dr. Lindeman. One of the orthopedic surgeons, Dr. Tom Green, adopted the boy, who was eight or nine at the time.”

Marguerite Mansperger, RN: Longtime Director of Nursing, School of Nursing
(Excerpted from “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”; Written by Gerry Shaver, RN, retired associate director, Nursing, Virginia Mason Medical Center)
“Marguerite Mansperger, RN – ‘Miss M’ to all who knew her – started working as a staff nurse at Virginia Mason in 1946. In 1947, she became director of Nursing Service and the School of Nursing. She once said that she had planned to work at Virginia Mason Hospital for only one year. She retired nearly 35 year later.
“Miss M grew up in Yakima, Wash. She received her nursing training from the School of Nursing at Seattle General Hospital. Although she earned a degree in nursing, she always rated a nurse’s ability to do the job above education level.
“When asked about honors or special recognition for her contributions to nursing, she would simply smile and say, ‘Girl, it was just my job.’
“Her integrity, compassion and leadership for excellence in patient care created an atmosphere that resulted in a fiercely loyal nursing staff. She always supported decisions made by her staff. She would give guidance, reprimands when necessary, and suggestions for better decisions, but, in public, always support.
“In 1975, Miss M retired to her lovely home in Maple Valley and an era ended. Many loyal friends are proud to have been associated with a nursing leader as distinguished as Miss Marguerite Mansperger, RN.”

Miss Mansperger (left) with fellow nurse Helen Kinnaman, RN.
Marguerite Mansperger, RN: Longtime Director of Nursing, School of Nursing
(Excerpted from “Vision and Vigilance: The First 75 Years, Virginia Mason Medical Center, 1920-1995”; Written by Gerry Shaver, RN, retired associate director, Nursing, Virginia Mason Medical Center)
“Marguerite Mansperger, RN – ‘Miss M’ to all who knew her – started working as a staff nurse at Virginia Mason in 1946. In 1947, she became director of Nursing Service and the School of Nursing. She once said that she had planned to work at Virginia Mason Hospital for only one year. She retired nearly 35 year later.
“Miss M grew up in Yakima, Wash. She received her nursing training from the School of Nursing at Seattle General Hospital. Although she earned a degree in nursing, she always rated a nurse’s ability to do the job above education level.
“When asked about honors or special recognition for her contributions to nursing, she would simply smile and say, ‘Girl, it was just my job.’
“Her integrity, compassion and leadership for excellence in patient care created an atmosphere that resulted in a fiercely loyal nursing staff. She always supported decisions made by her staff. She would give guidance, reprimands when necessary, and suggestions for better decisions, but, in public, always support.
“In 1975, Miss M retired to her lovely home in Maple Valley and an era ended. Many loyal friends are proud to have been associated with a nursing leader as distinguished as Miss Marguerite Mansperger, RN.”
SENSE Program by G. Ted Johnson, MD
(Excerpted from the book Virginia Mason Medical Center: The First 100 Years by Katherine Galagan, MD, and John Kirkpatrick, MD)
“‘Health Promotion’ was enjoying rising popularity across the nation [in the ’80s]. Patients and providers alike were interested in going beyond disease recognition and treatment to disease prevention and even further to creation of a sense of overall wellness. There was also speculation and hope that the cost of health care would decrease as lifestyle-related illnesses were prevented.
“Rather than develop its own, Virginia Mason purchased an existing wellness program from the Park-Nicollet Clinic in Minnesota. It was called SHAPE, but the Virginia Mason program was launched as SENSE, which was an acronym for the Satisfying Effects of Nutrition, Stress Management and Exercise.
“To launch the program and gain visibility, an intensive, four-day seminar at Rosario Resort on Orcas Island was offered to prominent local business leaders and their spouses. The weekend offered lectures, individual health assessments with physiologic measurements and blood tests, consultations on lifestyle and health, exercise sessions and healthy meals prepared according to the recipes in the SENSE cookbook. In addition to the information and experiences, participants were provided with motivational presentations and practical tips for setting goals and changing their current lifestyle habits into healthier ones. Each participant also received a shiny, polyester, navy blue exercise suit. It had a white stripe down the arms and legs and it became the work uniform for all SENSE team members.
“By that time, for reasons that now escape me, I had [become] medical director of SENSE. We added a variety of lifestyle-management courses to the quarterly calendar at Virginia Mason’s downtown campus. Each was a series of four to six weekly sessions. Our three primary programs were ‘Smoke Stoppers’ for smoking cessation, ‘Be Trim’ for nutritional and weight management, and a stress-management course that didn’t have a catchy name.
“Surprisingly to me, I became a popular banquet speaker. My most popular presentation, unimaginatively entitled ‘Your Lifestyle and Your Health,’ was the same talk with which I began our seminars. As the title suggests, it was an overview of current knowledge about lifestyle habits known to impact health. I also offered presentations on ‘Stress Management’ and ‘Humor and Health.’ In an attempt to retain audience attention, I used a fair amount of humor in these talks and, as a result, I got a regional reputation for being entertaining. Organizations looking for an informative speaker who was also funny found me by word of mouth, and I ended up giving hundreds of presentations at conferences, professional organization meetings, service organization lunches and even high schools.
“The fees generated by my presentations represented a small portion of our revenue, but the exposure often led to further programming and some individual enrollment in our various programs.
“I had a good time. I also ate a lot of mediocre banquet food. I don’t miss that at all.”

Duane Kesti
Virginia Mason Bainbridge Island and Virginia Mason Seattle
“If feeling that every person from the front desk to the procedure room cares and will do their best to help you get better matters, this is where you need to be. In comparison to other medical groups that I have had to deal with, this is so much better. I feel safe and confident that they are driven to do the best job possible. I hope Virginia Mason brings more of a presence to Kitsap County so the population here can have this kind of advantage in health care.”
Paul Fredlund, MD: Started practicing at Virginia Mason in 1975
(Excerpted from an interview on July 9, 2015)
“At the end of my fellowship with the National Institutes of Health (NIH), I wrestled with the idea … do I want to go into academic medicine for the rest of my career? Or, do I listen to my heart and practice medicine? Although I was offered a position at the NIH, I was looking for a place that allowed for academic rigor and the chance to care for patients. Virginia Mason fulfilled those goals and, as a bonus, it had great medical, surgical and anesthesiology residencies. I never would have gone into a position that didn’t offer the opportunity to interact with house staff.
“One day, I got a call from Dr. Bob Mecklenburg, who had been working with our group at the NIH. He was one year ahead of us in the fellowship and Bob had found what he said was nirvana … practicing medicine at the Mason Clinic in Seattle. I was immediately excited about the possibility. Shortly thereafter I came for interviews with Drs. Fritz Fenster, Dick Winterbauer, Jim Coatsworth and a whole cadre of fabulous physicians interested in academic care.
“I think the Surgical section was such a magical place to work. How many people get to spend their career working with best friends? It really was a family. My friend and colleague Dr. Jim Benson arranged my only blind date, which is how I met my future wife, Penny. I think the magic was that it was a completely supportive work environment. A patient who came to the clinic’s Endocrinology section effectively had six consults, rather than one.
“Although we weren’t part of the University of Washington, we all had joint appointments there. We would watch development happen in academic centers around the country and then try to translate it into actual patient care. In a 1985 issue of the New England Journal of Medicine, the lead article, which we wrote, showed for the first time that an insulin infusion pump had the long-term ability to maintain glycemic control.
“This would not have been possible without the help of nurse clinicians. Medicine depends on nurse practitioners and nurse clinicians … physician extenders. We came to that realization 25 years ago. In fact, it was largely because of collaboration between nurse clinicians and doctors that that article made it to the New England Journal.”
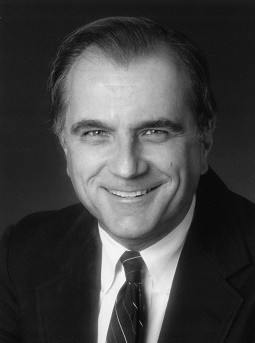
Transgender Health: Virginia Mason Providers Driven to Do this Work
Samantha’s steadfast advocacy for transgender health care first caught the attention of her Virginia Mason primary care doctor, who asked if she would join the guiding team working to develop Transgender Health services. Eager to be involved, Samantha applied to become a Patient-Family Partner (PFP), a unique volunteer program that invites patients and families to be active co-designers of the care patients receive.
In her new role, Samantha made an impression on the PFP clinical team: Would she be willing to share her personal story while presenting to the medical center’s Board of Directors?
“I told the board about both positive and negative experiences I’ve had,” said Samantha. “But Virginia Mason has these wonderful providers that really do care, they are driven to do this work. It’s so amazing to find that.”
Virginia Mason’s health equity work was already changing the organization when Samantha presented to the Board in September 2017. A renewed commitment to providing affirming care for lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ) people spawned system-wide improvements, from policies and staff training, to new care guidelines across medical specialties.
A face-to-face connection can open people to new ideas, a power that drives Virginia Mason’s Transgender Health service line guiding team. Providers from across the patient care spectrum – from clinical staff to administrators to physicians and surgeons – join with patient partners to learn from each other, as they work to improve the care experience of transgender patients.
Active goals for the guiding team include more staff education through facilitated discussions, creating a welcoming environment with everything from all-gender restrooms to affirming medical forms, and continued outreach to partner organizations and the LGBTQ community.
“This is a new frontier in medicine,” said Samantha. “I’m very proud of the giant step Virginia Mason has taken in this direction. They are passionate about equity in health care and making things better for people. It’s an exciting time.”

Don Wehmann
Virginia Mason Seattle
“I was born at Virginia Mason 66 years ago while my father was a student at the University of Washington. I still have my primary care physician and several other specialty care doctors at Virginia Mason. My 66-year relationship with Virginia Mason is testament to how much it has cared for and impressed me over the last six decades.”
Come back soon for more great stories as we celebrate our centennial.