Cancer Patient Stories
Virginia Mason Franciscan Health Cancer Care is deeply committed to providing the highest quality care for our patients, every day. We thank them for sharing their unique stories.
Patient story videos
Buck, esophageal cancer
Magdalena, bile duct cancer
Dana, breast cancer
Linda Fortune, breast cancer
Nancy, breast cancer
Shannon Wulik, breast cancer
Yvette Fosberg, breast cancer
Alan Roberts, colon cancer
Josephine, colon cancer
Sarah Davis, colon cancer
Waylon Kostrzewski, colon cancer
Yaffa Penski, kidney cancer
John Thompson, lung cancer
Kandi Mejia, lung cancer
Kathy Calvert, lung cancer
Peter Newcomb, lung cancer
Mary, pancreatic cancer
Scott Vanderflute and Kelly Bolender, prostate cancer
Wade, rectal cancer
Ron Goodnough, testicular cancer
Cancer patient stories
-

My name is Paul, and I was first diagnosed with cancer in 1996 when I was only 34 years old. I was in the Air Force and living in Germany. I worked in a military garage taking care of various vehicles. Back then we didn't use a lot of protective gear, even though we were exposed to all kinds of chemicals in the solvents and cleaning fluids we were using. Today, these things are known to cause cancer.
When I had my first symptom, I was young and active, in shape, and I had never smoked. I was married and had two kids. Life was good, and I felt fine. So it was a shock when I went to the bathroom one day to relieve myself and what came out was blood.
It blew my mind. I went straight to the hospital with my adrenaline pumping. I started to rationalize that it must've been something I ate because I didn't have any problems until that day. But that wasn't the case. I had bladder cancer.
In 1996, I had surgery, and the hope was that it would take care of the problem. It didn't, and because of my medical condition, I left the Air Force the next year. My doctor in Germany had connections to the Northwest and told me to see a particular doctor at Virginia Mason when I got home.
I was only back for five days when I found out that my mother's best friend worked for this doctor. The long story short is that I became a patient at Virginia Mason and today I can say that I’m a 20-year bladder cancer survivor. I truly believe without the care I received from my doctor and everyone at Virginia Mason, I wouldn't be here today. It seems everyone hates going to the doctor, but I don't. I look forward to it because the people at Virginia Mason make it a good experience.
Cancer can happen to anyone, but if you have the right people taking care of you, you don't have to be a victim. My belief is that challenges are good for you since you learn what you’re capable of doing. I've found that I'm capable of handling a lot.
To other cancer patients, I would say, "Get healthy, get strong, and develop a positive attitude. Find the right people to take care of you, and follow their instructions. Your body can do amazing things and you can get better, even after a diagnosis of a life-threatening condition like cancer."
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Loved ones also share in this difficult, life-changing experience. And the support they offer during this journey can make all the difference.
Just ask Burien resident Diana Dena and her husband, Andrew. When their lives were affected by a breast cancer diagnosis, they turned to our area’s best care at Highline Cancer Center.
Reminder call
A reminder phone call that it was time for her annual mammogram prompted Diana to perform an impromptu self-exam. She felt a hard lump and was immediately concerned—this lump felt different from benign lumps that had been discovered in the past. “Before I ever went in, I knew. Before the ultrasound and biopsy, I just knew,” she said. “I had cancer.”
Show of support
As Diana faced surgery and chemotherapy, she found support at every turn. “My husband was faithfully supportive; just a wonderful caregiver,” she said. Her daughters, Melissa and Rebecca, and two of Diana’s sisters also assisted in caring for her and taking her to appointments when Andrew had to work. Her 86-year-old mother and two other sisters shaved their heads when Diana’s own hair began to fall out.
Their church family also showed up. Between meals that arrived each evening and greeting cards that came every day, the outpouring of love is something Diana says touched her deeply and helped her to maintain a positive outlook.
The caring and supportive nature of the entire Highline team is something that struck Andrew. It was a stark contrast to their experience at a different hospital where Diana began treatment before transferring to Highline. “To this day, if we have questions, we call and get a good response. We are very, very thankful Diana received her treatment at Highline,” he said. “We believe through prayer God directed our path to Highline Oncology, Dr. Xie and the nursing staff.”
We’re in it together
The experts at Highline Cancer Center are here to provide you with clear information and to address any concerns. Our area’s expert team of oncology doctors, nurses and staff coordinates care to make sure everyone is on the same page. This means that starting from the moment we first see you and all the way through your treatment program, you get high-quality, compassionate care.
-
As a longtime health care employee, Dianne Munroe knows the importance of regular cancer screenings. During the three decades she spent as facilities director for Highline Medical Center, her mammograms were routine and uneventful.
When the time came for her regular mammogram in 2016, though, Dianne adjusted her routine. She opted to put her mammogram off for a few months while she waited for the highly anticipated 3D mammography technology that was coming to Franciscan Breast Center - Burien.
When Burien’s 3D mammograms became available, Dianne went in. She felt as healthy as ever, so she was surprised when the sophisticated imaging revealed a small cancerous lump in her breast.
Dianne’s breast cancer was caught early and hadn’t spread to other organs, but still required swift treatment. From there, Dianne says Highline’s medical community wrapped around her, ushering her through her diagnosis, answering her questions, and assisting with follow-up care.
Right away, Dianne saw Virginia Mason Franciscan Health surgical oncologist Dr. Ani Fleisig, MD, to discuss her options. Dr. Fleisig performed Dianne’s lumpectomy in September 2016. Soon after, Dianne started a month of radiation therapy at Highline Cancer Center. “My care was just excellent all around,” she says. “I didn’t know Ani Fleisig, but I had an appointment with her the next day, and I was treated like I was her most important patient.”
Today, Dianne’s good health allows her to enjoy her recent retirement and spend time caring for her mother, who also experienced early-stage breast cancer years ago. She encourages women to keep up with regular mammograms, even if they feel fine and have no reason to suspect cancer. “I would recommend Highline to anyone, and in fact, I do, all the time,” she says. “When someone I know needs a mammogram, I’ll tell them ‘Highline is right here, and they have everything you need.’”
“They have great care, great people, and great follow-up. They just do an excellent job.”
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Loved ones also share in this difficult, life-changing experience. And the caring support they offer during this journey can make all the difference.
Just ask Eileen Mosher, RN, MHA, who has worked at Virginia Mason Franciscan Health for more than 16 years. Her experience in operating rooms permitted her to witness Virginia Mason Franciscan Health’s skilled surgeons at work. When her routine mammogram detected a tumor, there was no hesitation—if she had to fight breast cancer, she wanted Virginia Mason Franciscan Health on her team. For Eileen and her family—her husband, Robert Freeby, and their two children, the journey began at Franciscan Cancer Center.
Gathering of support
Eileen and Robert’s family members were surrounded by support at home and at Virginia Mason Franciscan Health. Friends took turns helping with car pools to get the children to sports practices, and they made a schedule to determine who was bringing dinner to the family each evening. “They were enormously helpful,” said Eileen.
At Virginia Mason Franciscan Health, Robert was impressed by the level of compassion shown by Eileen’s treatment team. During chemotherapy, people from different departments would stop by to make sure everything was fine and to ask if they could be of assistance. “Nutritionists would stop by, pharmacologists would stop by, and other folks who were connected to the treatment would stop by to make sure everything was fine,” said Robert. “It was just an unbelievably caring and effusive network that opened up.”
Meeting you where you are
“It’s not mandatory, but it is extremely helpful to have a family member or friend available at appointments,” said Lynne P. Clark, MD, FACS, a surgeon on Eileen’s treatment team. “It should be someone with whom the patient is comfortable—so much information is shared, and sometimes the patient does not hear everything. So it is a way of checking information and also a sounding board when decisions need to be made.”
Not everyone is fortunate enough to have a strong support system. Virginia Mason Franciscan Health has services in place to offer assistance in every scenario. “Our support services do their best to help find the resources to assist patients through their treatments, from nurse navigators to social workers to many other people who work behind the scenes to assist cancer patients,” said Dr. Clark.
Nurse navigator Susan Nixon, RN, was there to guide Eileen and Robert as they prepared for surgery and recovery. “I had the mastectomy, a port placed and reconstruction—Susan came to see us every time,” said Eileen. Susan made sure they knew what to expect at every stage of treatment.
“Out of everybody we met with and spoke with, I never got the impression from anybody that they were only talking to Eileen about her diagnosis and prognosis,” said Robert. “They were talking to both of us from a very humanistic and holistic perspective.”
At Virginia Mason Franciscan Health, we’re in it together
After a cancer diagnosis, there is a lot of information to take in and decisions to be made. That’s why our experts are here to provide you with clear information and to address any concerns. Our area’s expert team of doctors, nurses and staff who specialize in cancer diagnosis and treatment coordinate care to make sure everyone is on the same page. This means that starting from the moment we first see you and all the way through your treatment program, you can expect high-quality, compassionate care.
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Spouses, children and loved ones also share in this difficult, life-changing experience. And the loving support they offer during this journey can make all the difference.
Just ask Gig Harbor resident Gretchen Beckman and her husband, Dan. When their lives were recently affected by a breast cancer diagnosis, Gretchen and Dan turned to our area’s best care at Jane Thompson Russell Cancer Care Center at the Milgard Medical Pavilion at St. Anthony Hospital.
An unexpected discovery
Gretchen was in the good habit of getting annual mammograms, and the most recent results were normal. But in December 2013, she felt a lump in her breast. She wasn’t even searching for it. “I took off my bra and just felt it. It was right there.”
Gretchen, with the support of her husband, saw her doctor the next day and was referred for another mammogram. Breast cancer was ultimately confirmed. Without hesitation she knew where to turn—her father had battled cancer, and she remembered how well the Virginia Mason Franciscan Health team treated him.
“It all happened pretty quickly,” Gretchen recalled. After a biopsy and other tests, her medical oncologist Frank M. Senecal, MD, FACP, medical director of Franciscan Cancer Center, decided the best course of action would be chemotherapy, then mastectomy, then radiation. It was going to be a long journey, but Dan was committed to being with Gretchen every step of the way.
Personal touch
Top-notch care is paramount, but personal interactions with doctors and nurses from Jane T. Russell Cancer Care Center are what confirmed for Gretchen and Dan they were in the right place. The couple found comfort in the relationship they built with the doctors and their staff. The team made sure both Gretchen and Dan had all the information they needed to make informed decisions, and they demonstrated genuine care and compassion throughout the entire process. “It’s just a small item, but all the providers always hugged my wife, and that made me feel good,” said Dan. “And they said ‘God bless you’ each time. We both have a strong faith, so that meant a lot to us.”
Gretchen also formed bonds with her chemo nurses. “I love all my chemo nurses,” she said. “If you have to go through chemo, I would rate the experience at the cancer center very highly.”
For Gretchen and Dan, their outcome was a happy one. Gretchen finished her final day of chemo on her 49th birthday surrounded by 14 family members and close friends.
Best treatment option for you
There are several types of breast cancer and many possible treatments. The team of experts at the Jane T. Russell Cancer Care Center will work with you to identify and explore all your options. You can count on them to be knowledgeable about the latest clinical trials and research.
To determine an action plan, it’s necessary to first identify the type of cancer present. A biopsy helps doctors check for estrogen receptor, progesterone receptor and HER2/neu receptor. These results help determine the appropriate treatment regimen since certain types of breast cancer respond well to some forms of treatment but not others.
Sometimes surgery is the next step after biopsy—surgery could mean a lumpectomy or mastectomy. In cases where the tumor is too big or aggressive, chemo is given before surgery. Clinical trials show that in aggressive tumors, especially in triple negative tumors, if chemo is given upfront, there is a better chance the tumor won’t return.
We’re in it together
After a cancer diagnosis, there is a lot of information to take in and decisions to be made. That’s why our experts are here to provide you with clear information and to address any concerns. Our area’s leading team of doctors, nurses and staff coordinates care to make sure everyone is on the same page. This means that starting from the moment we first see you and all the way through your treatment program, you get high-quality, compassionate care.
-

When Heather Steffenson was in her mid-40s, her primary care physician asked her why she wasn’t getting yearly mammograms. She replied that she didn’t have a family history of breast cancer and wasn’t worried. “My doctor said, ‘Well, someone has to be the first in the family.’ That always stuck with me,” said Heather, now 52.
Since then, Heather never missed a yearly mammogram. But in 2018, she postponed her annual appointment for several months. “I was turning 50 in October and wanted to do all my screenings that I’d need at the same time,” she said.
In October, she had a mammogram at the Franciscan Breast Center – Burien, and was called back a few days later for a second screening. On November 7, she received her diagnosis of breast cancer. At just 1.2 centimeters, her tumor was small and early stage. But because Heather’s cancer was HER2-positive, it was more aggressive and would require a longer course of chemotherapy.
Right away, Heather met with Virginia Mason Franciscan Health surgeon Ani Fleisig, MD, and an oncologist. A few weeks after her lumpectomy, Heather began a 14-month course of chemotherapy and radiation. She credits her personal support network and her Virginia Mason Franciscan Health care team for helping her manage her symptoms and continue many of her normal activities during the lengthy treatment.
“People ask me all the time how I got through it. I tell them you have to have an absolutely tremendous support team, and I did. My husband, Paul, was my rock, and Dr. Fleisig, Dr. Patel, the nurses, and the radiation techs at Highline were so spectacular,” Heather said. “I would recommend Highline to anyone going through this.”
Being able to receive treatment at Highline Medical Center, just 15 minutes from her home in Des Moines, helped Heather maintain a normal routine and continue working full time during treatment, she said. “A lot of people have asked me why I didn’t go to a downtown hospital. I just don’t feel like I could have had better care than what I had here at Highline. It’s been a fantastic experience.”
On March 11, 2020, Heather had her chemotherapy port removed and returned to her active lifestyle of cycling, hiking, kayaking and cheering for the Seattle Mariners. She served as the Mariners’ Honorary Bat Girl for the Breast Cancer Awareness game on May 17, 2020. Helping encourage others to care for themselves is an honor, she said.
“It's so easy to get wrapped up in your life and forget to take care of yourself, but I’m a walking billboard for breast cancer screening,” she said. “I tell everyone I meet not to skip their annual mammogram.”
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Loved ones also share in this difficult, life-changing experience. And the caring support they offer during this journey can make all the difference.
Just ask Sumner residents Heidi Geise and her husband, Paul. When their lives were affected by a breast cancer diagnosis, Heidi and Paul turned to our area’s best care at St. Francis Breast Clinic.
The power of a routine exam
Heidi was diagnosed with breast cancer at age 57 after a routine annual mammogram. Her gynecologist referred her to the cancer multidisciplinary team at St. Francis Breast Clinic—a move that Heidi looks back on with gratitude. “I appreciated the way they worked with me and helped me to deal with the fact that I had just been diagnosed with something that wasn’t good,” she said. “I felt like they were taking care of me. It was the right place to be.”
Heidi’s husband, Paul, was by her side during the six-month treatment process, which included surgery and then chemo at St. Francis Hospital and breast reconstruction at St. Joseph Medical Center. Paul was tasked with bringing a notepad to appointments so they could write down the doctor’s responses to questions he or Heidi asked. “You want to know what’s going on, and they didn’t hold anything back,” he shared. “They said, ‘This is what’s going to happen, but you will get through it.’”
The situation was unfamiliar. But Heidi’s treatment team guided the couple through the process. “I trusted the doctors,” said Paul. “They knew what they were doing, and they attacked the problem. There was no waiting around. It was ‘Let’s get this done. Let’s take care of this and get you back on recovery.’ I was duly impressed with that.”
The couple’s son, John, was away at college when his mom was diagnosed. Through frequent phone calls, his dad relayed information and kept him up-to-date with how treatment was progressing. His parents’ confidence in the Virginia Mason Franciscan Health team eased some of the anxiety and made a difficult situation more bearable.
A team approach
The team works together in a multidisciplinary function to explore all options and ensure the best possible care. Heidi appreciated the team’s communication. “Everyone knew what everyone else was doing. I didn’t have to worry about whether or not one person was doing something that another person wouldn’t know about, or worry about whether or not something would be approved,” she said. “They were a team working on my team.”
At Virginia Mason Franciscan Health, we’re in it together
After a cancer diagnosis, there is a lot of information to take in and decisions to be made. That’s why the experts at Virginia Mason Franciscan Health are here to provide you with clear information and to address any concerns. Starting from the moment we first see you and all the way through your treatment program, you get high-quality, compassionate care and follow-up.
Cancer care at Virginia Mason Franciscan Health is provided by expert network partners, including Virginia Mason, Northwest Medical Specialties, Tacoma Radiation Oncology, TRA Medical Imaging, and the Puget Sound Institute of Pathology.
-

Tacoma resident Joleen LaMay is known for her energy and positive outlook on life. A Sumner High School health and fitness teacher and assistant women’s basketball coach at the University of Puget Sound, Joleen has the will and drive of an athlete. In the last year, these strengths helped her through one of life’s most difficult challenges: cancer.
Now 47, Joleen had her first mammogram at 35. She learned then that her breast tissue was dense and fibrous. She did regular self-exams, but never made it back in for her next routine screening mammogram.
“For 10 years, getting a mammogram stayed on my list of things to do,” Joleen says. Last August, she decided finally to schedule the test. Ironically, just a few days later, she felt a large, hard, alarming mass on her breast as she was getting into the shower. “I googled it, of course. I knew it could be cancer, but it could be many other things, too.”
Joleen immediately made an appointment with her primary care physician, who was clearly concerned. “My doctor sent me to Carol Milgard Breast Center right away for my mammogram. I still thought it was probably ‘one of those other things’ and not cancer,” she says. “Then I had a second mammogram, an ultrasound and a biopsy, all at Carol Milgard.”
Then the results came back. “I remember hearing, ‘This is not the news we wanted to share with you.’ It was August 18. My life changed that day.”
Where to turn when life takes a turn
After the diagnosis, Joleen asked her nurse to help her choose an oncologist. “I asked who she would want, if it were her, and she told me about Dr. Senecal.”
Frank Senecal, MD, Northwest Medical Specialties, is part of the multidisciplinary team under St. Joseph Medical Center’s breast cancer program. “The crew in that office is absolutely amazing,” Joleen says. “They look after you. They care for you. They are kindhearted and warm. I often reached out to Dr. Senecal and Debra Morris, ARNP; they were so available to me.”
“It’s such a huge ordeal to be diagnosed with cancer,” Joleen says. “Chemo is scary and difficult and hard to manage. I knew discomfort and physical challenge—I’ve been an athlete all my life. But this was on a whole different level.”
Joleen was grateful to have advanced treatment available close to home; this allowed her to stay at work. “It gave me the ability to continue teaching and coaching throughout my treatment,” Joleen says. “One day I remember going to chemo in the morning and sitting on the bench coaching basketball at Puget Sound that night. The convenience of close to home makes it easier to manage the little things.”
A close friend who had recently completed breast cancer treatment helped her prepare for the unexpected, and her family and friends rallied in countless ways. Joleen didn’t turn to the cancer program’s support groups, but she would have if she’d needed to. “My advice to others going through this is, don’t hold it in. Reach out. You don’t want or have to do it alone. Cancer is too big a monster to do it by yourself.”
Joleen’s treatment lasted nine months—from diagnosis on August 18 to her final radiation treatment on April 20. She’s now cancer-free.
“You feel you won’t get through it, but you do,” she says. “Here I am.”
The value of inclusive care
The breast cancer programs at St. Anthony and St. Francis hospitals and St. Joseph Medical Center are fully accredited by the National Accreditation Program for Breast Centers (NAPBC). These programs provide the best possible patient care by consistently meeting or exceeding NAPBC’s stringent guidelines and national quality standards. Patients can expect to receive the most advanced treatment options without having to travel outside the region.
The inclusive care provided at these locations allows women with breast disease to go from screening mammography to a complete diagnostic work-up in one place. While most women will never need the full range of services offered, the few who do have the comfort of knowing they are in the most capable and qualified hands. Multidisciplinary teams of specialists (cancer surgeons, medical and radiation oncologists, navigators, and others) collaborate with patients to provide the best possible treatment plan while minimizing the time from finding a breast concern to diagnosis and treatment.
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Spouses, children and loved ones also share in this difficult, life-changing experience. And the caring support they offer during this journey can make all the difference.
Just ask Lake Tapps residents Kerie Swepston and her husband, Aaron. When their lives were affected by a breast cancer diagnosis, Kerie and Aaron turned to our area’s best care at Virginia Mason Franciscan Health.
An unexpected discovery
An annual exam at age 45 didn’t sound any alarms for Kerie. She received a clean bill of health. Her doctor gave her a referral for a mammogram since she was due, but Kerie felt fine and didn’t see a need to rush to schedule the appointment. The doctor had performed a breast check during the exam and there were no lumps, and Kerie hadn’t felt anything suspicious during previous self-exams.
That changed a month later when her hand brushed against a lump while she was undressing one evening. She went to Aaron and had him feel it too. He agreed—it didn’t seem normal. They decided she should have it checked. After a mammogram and subsequent biopsy, Kerie learned she had breast cancer.
Better care and communication
Kerie and Aaron became frustrated as they attempted to connect with various specialists at another hospital. They had been told that the type of cancer Kerie had was aggressive, but they were having difficulties getting appointments to be seen right away. Luckily, Kerie’s primary care physician saw how things were progressing and referred her to Sibel Blau, MD, a medical oncologist at Northwest Medical Specialties/Rainier Hematology-Oncology in Puyallup.
Kerie was surprised—and delighted—to learn that Dr. Blau wanted to see her the next day after regular business hours. “To me that said, ‘We are taking care of it right now,’” Kerie said.
As his wife began treatment, Aaron had lots of questions. Dr. Blau helped him find his footing by explaining what he could expect. “Dr. Blau is brilliant, but she doesn’t talk like an academic. She uses layman terms so you understand everything. And it wasn’t like I was bothering her to get questions answered that she has answered for every other patient. She answered every question as if it was a fresh question,” he said. “She helped take away some of the fear by eliminating the mystery.”
More treatment options
Dr. Blau is involved in and familiar with current breast cancer research. “We have clinical trials available to our patients; this means new drugs that aren’t normally available that patients can access. We have a much bigger program than other hospitals, and we have a continuity of care that is incredible,” noted Dr. Blau. “I think that’s what makes us special.”
At Virginia Mason Franciscan Health, we’re in it together
After a cancer diagnosis, there is a lot of information to take in and decisions to be made. That’s why the experts at Franciscan Cancer Center are here to provide you with clear information and to address any concerns. Our area’s leading team of doctors, nurses and staff coordinates care to make sure everyone is on the same page. This means that starting from the moment we first see you and all the way through your treatment program, you get high-quality, compassionate care.
Cancer care at Virginia Mason Franciscan Health is provided by expert network partners, including Virginia Mason, Northwest Medical Specialties/Rainier Hematology-Oncology, Tacoma Radiation Oncology, TRA Medical Imaging and the Puget Sound Institute of Pathology.
-

When Luciana Bosio was diagnosed with breast cancer in 2018, she was surprised at how calm she felt. The news was certainly upsetting, especially for the people who love her. But her immediate response was to develop an action plan, and for that she turned to Virginia Mason Franciscan Health.
“The moment I was diagnosed, I had a team to care for me,” she said. “The surgeons, doctors and nurses were amazing—supportive and reassuring, but not patronizing. I didn't want to be treated like I was sick. It was important to me to be treated like a person who had a problem at the moment and needed help with that problem. They always listened to me and always included me in the planning.”
Fortunately, Luciana has long been committed to getting an annual mammogram, and her cancer was found early. That gave her the option of having a lumpectomy rather than a mastectomy to remove her entire breast. Surgery successfully removed the cancerous mass, and the margins around it were found to be clean.
Chemotherapy was then recommended to reduce the risk of recurring cancer. Luciana said no. She didn't want to be sick or have her hair fall out, or any of the other side effects she associated with chemo. But she did agree to talk with Nanette Robinson, MD, an oncologist at Virginia Mason Franciscan Health.
“The first time I saw Dr. Robinson, I told her I wasn't going to be doing any chemo and I wasn't going to be doing any radiation,” she said. “I didn't want anything like that.”
Luciana is a strong-willed woman, but found she’d met her match in Dr. Robinson.
The oncologist listened to her concerns, and then explained new developments in chemotherapy. She shared data that showed how chemo could dramatically reduce Luciana's chances of cancer coming back. And she suggested CMF—a combination of drugs that are milder than other chemotherapy drugs but taken over a longer period of time. Luciana accepted the challenge, and for 24 weeks, she came to Virginia Mason on Fridays for a CMF injection.
Her husband, Pedro, was with her for every injection. Luciana and Pedro have been together most of their lives, since their first crush at ages 13 and 14. Originally from Argentina, they've been married almost 25 years. They work together as well, as radio producers for the Marty & Jodi show on 95.7 The Jet.
Both are grateful to iHeart Media Seattle for being incredibly supportive. Staying active in her job helped Luciana stay focused. She was determined to stay positive, and a work environment full of fun and laughter helped her keep her sense of humor as well.
Although Luciana was often tired, and occasionally had bouts of mental fuzziness (typically called chemo brain), she never got sick during treatment, and her hair did not fall out. She was still able to work, do yoga every day—and even travel to Argentina to visit her family.
“I have to tip my hat to Dr. Robinson for convincing me to do something I didn’t want to do,” Luciana said.
-

I’m Linda, and I'm 68 years old. Three years ago, I was diagnosed with breast cancer. When I had my regular mammogram, something didn't look right. They wanted me to come back for another mammogram and ultrasound. That showed a possible tumor, and a biopsy revealed I had cancer. I also had an MRI that gave them a better picture of what was there.
Luckily, it was Stage 1A HER2 positive, and I wasn't in immediate danger. But I felt like everyone at Virginia Mason took it just as seriously as if it had been Stage 4. A meeting was quickly set up for me to talk to an oncologist, radiologist and surgeon. I felt that each one focused on me as a person, on my particular cancer and how it might be treated. They answered all my questions.
I decided to have a lumpectomy, and that went well. I had a one-time intraoperative radiation treatment and was only in the hospital overnight. I did have some problems with the follow-up treatment because my wound was proving difficult to heal. It was a couple of months before I was able to receive chemotherapy once a week and had some difficulties with that, but a nurse was always available for me to talk to.
One of the oddest things was that I didn't like the taste of silverware during my treatment. So I had to eat every meal with plastic utensils. But the good thing was that I didn't eat as much and lost 55 pounds. I love to cook and bake, and I knew I was too heavy.
Today, I am eating much better, and I feel better because of it. I have rheumatoid arthritis and I need to stay active, so I exercise by doing water aerobics. My family has been terrific through all this. When I was in treatment, my sister-in-law would visit every Tuesday. She knew I wouldn't be feeling well that day because of the chemotherapy, and she would bring me things I could eat.
Just recently, my daughter, Traci, was diagnosed with breast cancer. When she found out
about it, she knew immediately she wanted to be treated by the same doctors at Virginia Mason who treated me. It was also recommended that she visit Virginia Mason’s genetic counselor—and we went together.
I learned a lot from that visit. When you look at the big picture, you can see how cancer has affected my family through generations. I suppose that's true for a lot of families, but it was surprising to realize how many of my relatives have had cancer.
I'm so glad that Virginia Mason was there for me and Traci. And in 2005, it was there for my husband, Otis, as well. He had prostate cancer and is doing well today—and so am I. Otis, Traci and I have all had the best care possible. I can't say enough good things about the people at Virginia Mason who took such good care of us.
-

About 1 in 8 women will battle breast cancer. But many more lives are affected. Loved ones also share in this difficult, life-changing experience. And the caring support they offer during this journey can make all the difference.
Just ask Puyallup resident Maggie Eastman and her family. She felt a lump in her breast during a self-exam on her birthday. There was no family history of cancer, and at age 32 she thought she was too young for something as serious as breast cancer. When two mammograms and two ultrasounds came back as inconclusive, it was time for the next step. Her family gathered around her as she continued to search for answers.
Family support
Maggie was referred to Lynne P. Clark, MD, FACS, a surgeon who specializes in breast cancer at Franciscan Surgical Associates in Tacoma for evaluation. At Maggie’s initial appointment, Dr. Clark felt a biopsy should be done even though the mammograms and ultrasounds were inconclusive. The biopsy was done immediately in her office. When the results were in, breast cancer was confirmed.
Maggie’s parents, her brother and her sister participated in her treatment from the beginning. “I’m very lucky to have a wonderful support system,” she said. “My family was in the room when my doctor told me I would have to have a mastectomy. To have them there, willing to hear the details without shying away, was enormously helpful.”
Maggie’s dad, Rick, was at every appointment. “From our perspective as parents and caregivers, Dr. Clark is an amazing lady. Her capacity for compassion, and at the same time getting right to the point, is pretty amazing. She can put you at ease and makes sure you understand both the seriousness and scope of what’s going on.”
Dr. Clark’s entire staff helped make the difficult experience as bearable as possible by consistently demonstrating their dedication to Maggie’s well-being. “The nurses connected with Maggie on a level you can only hope for,” said Rick. “It was obvious they cared about her.”
Better care
Dr. Clark’s approach to communication meets you right where you are. “I feel it is important to treat patients as individuals and respect them for their journey and what they are going through,” said Dr. Clark. “This journey is too important, and many times life-changing, to put a rush job on an appointment. I feel there is a need to take the time necessary to help my patients understand what is happening in their body and how we can best treat it.”
Maggie will forever be grateful for the relationships she developed with Dr. Clark, her nurses and staff. “I didn’t realize it at the time, but I have since talked with people who have gone through cancer treatments at other hospitals, and they have been amazed at the level of compassion I’ve been shown—in addition to the great care I’ve received.”
At Virginia Mason Franciscan Health, we’re in it together
After a cancer diagnosis, there is a lot of information to take in and decisions to be made. That’s why the experts at Franciscan Cancer Center are here to provide you with clear information and to address any concerns. Our area’s leading team of providers, nurses and staff coordinates care to make sure everyone is on the same page. This means that starting from the moment we first see you and all the way through your treatment program, you can expect high-quality, compassionate care.
-

My name is Patti, and I'm 52 years old. I am social, outgoing, outspoken, a little ornery, kind and loving. I think the ornery part made me a GREAT breast cancer fighter!
I have been married to the man I love for 30 years! We have two adult children who choose to hang out with us, so I think we did a good job as parents. I also have horses, cats, chickens and a new dog. Today, my life is kind of awesome.
But in November 2011, a not-so-wonderful thing happened. I got a call I will never forget. My recent mammogram showed an area of concern. The biopsy I had a week later confirmed that I had breast cancer. When the nurse called to talk to me about the results, I jokingly said, "You're going to ruin my cleavage, aren't you?" I'm glad I have a bizarre sense of humor because it helped me so much in the months to come.
Within two hours of that first call, the nicest woman phoned saying she had everything scheduled, like the way travel agents used to do it all for you—one-stop shopping. It was so comforting to have someone be so helpful. I did get a second opinion, but ultimately chose Virginia Mason where my treatment went as smoothly as possible.
That's not to say there weren't challenges. For one thing, a genetic test showed I was positive for the BRCA1 gene mutation. In addition to breast cancer, mutations in the BRCA1 gene also increase the risk of ovarian and fallopian tube cancers.
I was not ready to make the choice for a mastectomy, so I talked through my options with my surgeon and went for an aggressive oncoplasty. This is where the breast cancer surgeon removes a lot of breast tissue to ensure the cancer is completely gone, then—during the same surgery—reconstructs the breast. At the same time, a plastic surgeon performs surgery on the other breast to make sure that both breasts are the same size and look good.
In other words, I got a bilateral breast reduction and came out of my cancer with one breast surgery and two beautiful breasts. Other doctors—not at Virginia Mason—told me I would have to have breast cancer surgery and then later a plastic surgeon would try to fix the missing breast to match. Virginia Mason is the only breast cancer program in the region to perform this type of oncoplastic surgery, so it was an easy decision for me. I could not afford that much time off work as a private business owner.
A month later, I went on to have a total hysterectomy per my choice because of the BRCA1 mutation. Five weeks later, I started bleeding. I kept thinking, "Now what?" Because I had bruised more than normal during my biopsy and surgery, my breast surgeon decided to test me for a bleeding platelet disorder. She discovered that this was what was causing the problem, and we resolved it.
I am here three years later cancer-free knowing she did a great job. I still miss my triple D bras every now and then, but buying a cute B cup bra is so much easier; so is jogging and horseback riding!
My surgeon and the Virginia Mason team that took care of me were simply the best, and their team medicine approach was a comfort. And my family and friends really stepped in to help when I needed them. My best friend, Jenny, came all the way from California and slept in my room for both my surgeries.
I had several breast cancer survivor friends who helped me understand what I was feeling. They are the reason I now go out and help other women who are facing this for the first time. My own kids and my day care families cooked and cleaned and made sure my day care business stayed open without a hitch.
My life is definitely different because of cancer. For one thing, I realized I was not living to my full potential. I got that horse farm I always wanted, and I fell in love all over again with my husband.
There were hard parts, but for me, the hardest was some people's reactions. I lost a few so-called friends, you know the ones who I was there to support but who could not see me sad or not fun. I miss them at times, but count myself lucky because I found out who was a real friend and who was not.
I know that the reality of my life today is that the BRCA1 gene mutation is in my family and can affect my children, siblings, nieces, nephews, and any grandkids I might have. So now I'm a fighter for all of us. I participate in fundraisers for breast cancer research, and I visit with and help women who are facing the same things I've faced.
The best thing about my life today is that I'm living it to the fullest. I think the next update from me will be about my daughter's beautiful wedding or maybe even grandbabies. I plan to be around for a very long time!
-

I’m Traci, and I recently learned I have breast cancer. Only three years ago, my mother, Linda, was diagnosed with breast cancer. I'm only 45 years old, and it was a little strange at first to have the same diagnosis as my mom.
I first found out I had a problem when I went in for my annual mammogram and got a call to come back. I wasn't worried because I've been called back before. I know there are areas on my mammograms that are sometimes hard to read. So I wasn't too concerned.
But this time they also did an ultrasound and asked me to wait for the results. I was surprised when they came out and asked me to make an appointment for a biopsy. This was done a few days later, and it showed I had cancer.
It was upsetting to get that phone call, even though the nurse was the nicest, most reassuring, person in the world. I already knew that I wanted to receive my treatment at Virginia Mason. I told the nurse I wanted the same surgeon, oncologist and radiologist who had treated my mom. Later that day, she called back to confirm that these would be the doctors handling my case.
My first meeting with them was really good. I was impressed by the way they addressed my concerns and that they made a tape recording of our meeting. I didn't need to worry about remembering everything that was said. When you're dealing with cancer, it can be hard to stay focused on the information you're getting. The tape recording told me that they were looking at things from a patient's point of view.
Because there's a history of cancer in my family, it was suggested that I see Virginia Mason's genetic counselor. My mom went with me and was able to fill in a lot of the information I didn't have. I learned that there is cancer on both sides of my family, and that I probably have a genetic predisposition for it.
I'm a surgery scheduler for another medical center, and one more thing I liked about Virginia Mason was that the schedulers made sure my appointments were at times that were the least disruptive to my work.
As I write this, my diagnosis is so new that I haven't yet had surgery. But thanks to my meetings with the people who will be taking care of me, I know that the lumpectomy will take about two hours in the morning, and then I will be able to go home that same afternoon.
I am so comfortable with getting my surgery and follow-up care at Virginia Mason. I know I will go in for my operation, return home and get back to normal. I consider myself lucky.
-

Veterinarian Dr. Chris Eugenio of University Place got his first colonoscopy five years ago at age 46, because his father and uncle have had colon cancer. That scan came back clean. The active, healthy dad of two expected the same for his second colonoscopy on September 17, 2018. This time, though, the results were different: Chris had a softball sized tumor nearly blocking his colon.
After his colon cancer diagnosis, Chris said he “cried for eight days straight, more for my wife and kids than myself.” On September 25, 2018, his tumor was removed by Virginia Mason Franciscan Health colon cancer surgeon Shalini Kanneganti, MD, at St. Joseph Medical Center.
Though his diagnosis was devastating, follow-up tests brought good news: Despite the tumor’s large size, the cancer hadn’t spread to other organs and was highly treatable. Chris opted for oral chemotherapy with Virginia Mason Franciscan Health oncologist Jorge Chaves, MD.
Currently on his third round of chemotherapy, Chris said he feels a bit tired, but otherwise healthy. Working closely with Dr. Chaves and a naturopathic physician helps him manage side effects and keep his energy up, and he’s still able to care for patients at Fircrest Veterinary Hospital, the local clinic he owns.
Overall, he said, he’s grateful to be alive. “Colon cancer is the silent killer, because I felt great,” he said. “I didn’t have symptoms, but my colon was in severe danger of rupturing. But because we caught this in time, I’m still here for my wife and kids.”
He encourages friends, family and veterinary patient parents to get a colonoscopy screening, sooner instead of later. “Please, get a colonoscopy,” he said. “If you have a history of colon cancer in your family, do it early. Start at 40. I’ve been telling all my friends, if you haven’t had one, please go get one.”
“If you’re going through this, it really does help to have a great support system and try not to do it alone,” Chris added. “We have a great community of support around us, and it made a huge difference. If you ever find you have cancer, reach out to people around you. It’s made a big difference.”
-
In 2016, Joe Goode of Eatonville was raising three active boys with his wife, Sarah, and taking college courses in accounting. When the active, healthy 46-year-old started experiencing abdominal cramps, constipation and bleeding, he chalked his symptoms up to a possible internal hemorrhoid. But a colonoscopy performed by Virginia Mason Franciscan Health gastroenterologist revealed a large tumor nearly blocking his colon.
The scan couldn’t be completed because the tumor was too large. "It was a shock, because I hadn’t even felt sick. I was really at the edge of a cliff and had no idea,” Joe said.
Joe’s diagnosis of stage 4 colon cancer meant he’d need treatment right away; his cancer had spread to his liver and lungs, and his colon couldn’t function properly with the blockage. His Virginia Mason Franciscan Health care team performed multiple surgeries at St. Joseph Medical Center in Tacoma, including a complex surgery in August 2016 to remove his colon tumor along with 70 percent of his liver.
Between surgeries, he received targeted chemotherapy and radiation therapies from oncologist L. Katherine Martin, MD, and radiologist Dennis Wang, MD, to shrink the cancerous tissue.
During his chemotherapy, Joe’s three boys picked up the slack at home, he said. “My oldest was then 12, and he would help his brothers get ready for school, make breakfast, and help any way he could. We had family and friends in the area so the boys could continue playing sports. I felt very supported.”
Joe’s Virginia Mason Franciscan Health care team expanded his circle of support, he said. “My Virginia Mason Franciscan Health doctors saved my life. I never felt like I was just a number; they really wanted to see me beat this. You become part of a team. They’re all caring, loving, very kind people, and the skills they have are amazing. They are definitely blessed, and a blessing.”
Today, he’s a strong advocate for colonoscopy screening. “Don’t wait to get it done,” he said. “Don’t wait until you don’t feel good—I didn’t feel anything, and I was at a stage 4. You’d think someone at stage 4 would be sick, but I didn’t feel sick. If I’d waited until I did, I might not be here.”
“Talking about colonoscopy can be uncomfortable, especially for guys, but there’s nothing to be uncomfortable about,” Joe noted. “The process is easy. You’re very comfortable and relaxed, then you wake up and get your results. You just have to take a day off from work, and that day off can save your life.”
-
Valerie Schock, local nurse, had no family history of colon cancer and was given a clean bill of health following her first colonoscopy at age 51. Soon afterward, though, she developed new gastro-intestinal symptoms like diarrhea and cramping. She sought medical help for these symptoms and was diagnosed with lactose intolerance. When she searched for an explanation for this condition, which seemed to develop suddenly, she was told that it was normal to develop some new food intolerances in mid-life.
Finally, after suffering with these GI symptoms for more than four years, she scheduled another colonoscopy for December 2016. This time, the colonoscopy revealed a 4 cm tumor in her colon. Valerie chose to receive treatment with Virginia Mason Franciscan Health under Shalini Kanneganti, MD, FACS, FASCRS, medical director of colon and rectal surgery at Franciscan Medical Group.
She began oral chemotherapy treatment to shrink her tumor in January 2017. By April, her tumor was small enough to be removed, and her surgery took place April 20, 2017. In May, she began intravenous chemotherapy, and in October 2017, she had a surgery to reverse her ileostomy.
Today, she still has her chemotherapy port, pending a follow-up visit with Dr. Martin. “As a nurse, I know the importance of screening, and I wish I hadn’t waited more than four years to go and get another colonoscopy. Screening is so important. The prevention of disease is so much easier for the patient if they catch things early. Listen to your body.”
-

During a routine exam, my doctor recommended I get a colonoscopy and endoscopy. So I scheduled those tests. The colonoscopy came back normal, but the endoscopy showed a mass in my esophagus that turned out to be cancerous. I had radiation and chemotherapy followed by surgery. I encourage all my friends to visit their doctor. I felt like a million bucks before the diagnosis and never would’ve known I had cancer if I hadn’t been screened. The cancer is now gone.
-
I’m James, and I'm 65 years old. For the past 36 years, I've worked for The Seattle Times, where I am a state area manager in circulation and responsible for covering one-third of the state of Washington. I'm married to Sheryl and have five stepchildren.
My family is wonderful. I've always had a great job, and for many years, I didn't have any serious health problems. But 10 months ago, I was diagnosed with esophageal cancer. Today, I can say I'm a survivor of this terrible disease thanks to the care I received at Virginia Mason.
It all started a while back when I kept coming down with pneumonia. I would get treated, and it would clear up, and then it would be back. Just before Christmas in 2014, I had to call 911 because I was having so much trouble breathing. They took me to a hospital on the Eastside where I live, but the doctors there could not figure out why I was having this problem. They did X-rays and saw blotches on my lungs, but since I had pneumonia they weren't concerned about them. While they treated me for the pneumonia, they kept looking for what was causing it.
I think it was the third time I got X-rays that they spotted something that didn't look right. They put a scope into my lungs but didn't see anything. My care at that point wasn't being handled very well. I was told that when I went home, it was OK for me to eat solid food. When I did, I started choking so badly that we had to make another 911 call, and I spent more time in the hospital.
This time, they did a “swallow” test where they watch as liquid goes down the esophagus. From this test, they could see a tiny bit of liquid leaking into my lungs. This leakage was probably what was causing the pneumonia. They put me to sleep and did an endoscopy, where they use a scope to look inside the esophagus. That's when they found I had a large tumor.
Even without getting the results of the subsequent biopsy, my doctor was certain I had cancer. He said that I would probably need a complex operation on my esophagus to remove the tumor and that there was a doctor at Virginia Mason who had done 800 of these operations.
I did my own research and agreed with him that that's where I needed to go. I am so glad I became a Virginia Mason patient at that point. I think it saved my life. I know two people who were treated for the same type of esophageal cancer, but not at Virginia Mason. Neither of them are alive today.
I had confidence in my Virginia Mason surgeon from day one. Everything was thoroughly explained to me, so I was ready. The operation lasted more than seven hours, during which the cancerous tumor was removed and a new esophagus built from my stomach.
I was in the hospital on a feeding tube for 12 days. Every person who took care of me was great. That was last October. I was back to work part time in February, and full time about a month later. In addition to the surgery, I had chemo and radiation treatments. When I had my first PET scan recently, there was no sign of cancer at all.
I was so impressed with my care at Virginia Mason that I plan to become a volunteer. I want to give back and maybe help other cancer patients like me.
-

For more than 20 years, Georgia Hartness did what she loved best: taught primary school on Vashon Island. According to a Vashon Island School District newsletter, by the time she retired in 2008, she had risen to the ranks of one of the “all-time greats” in the eyes of many of her fourth graders, thanks to her inspired curriculum and a creative birding program that incorporated science, art and writing.
Georgia's ability to excel at teaching is especially impressive because during this time, she was plagued with leukoplakia, an oral lesion that caused her tongue to be inflamed and made talking painful. “It was very discouraging,” she recalls. Her recovery took a long time and was very challenging. But what kept her going were her “great Virginia Mason doctors,” Stephen Bayles, MD; Kas Badiozamani, MD; and Prakash Vishnu, MD.
By the time she came to Virginia Mason in 2006, Georgia had already endured 19 years of treatment. Each time she had seen her previous doctors, they biopsied her tongue, but the plaque and the pain remained. She realized she needed doctors who were more knowledgeable and could find a way to control the plaque and save her tongue. So in 2006, Georgia had her first visit with otolaryngologist Dr. Bayles. Right away she knew she’d done the right thing. “I knew I was in good hands. He really listened to me and knew what I needed,” she remembers.
Four years later the plaque on her tongue changed and became more painful. New biopsies indicated cancer. Dr. Bayles excised the tumor, then radiotherapy began with radiation oncologist Dr. Badiozamani.
“Georgia came in every day for the next seven weeks for radiation therapy for her head and neck,” says Dr. Badiozamani. “The treatment is very tough. It can cause blisters on the tongue and makes swallowing very painful, but she remained really positive and motivated.”
While radiation therapy was going on, she also came in once a week for chemotherapy with Dr. Vishnu, who praises her for her bravery during the seven-week period.
In 2011, the cancer spread to a lymph node in Georgia's lower neck. Dr. Bayles removed the tumor and she returned to Drs. Badiozamani and Vishnu for another course of radiation and chemotherapy.
“It's always hard on patients when there is a recurrence. But even with the side effects, Georgia was graceful throughout and kept to the program,” says Dr. Vishnu.
In 2012, tests indicated she was finally free of the cancer. She has remained cancer-free and returns twice a year for follow-up appointments.
“It makes my day to see Georgia feeling good,” says Dr. Badiozamani. “She's an amazingly resilient person,” adds Dr. Bayles.
Georgia feels blessed by her experience at Virginia Mason. “How can you think that you'll go to the hospital for cancer treatment and wind up with three wonderful doctors who you like and respect?” she asks. “I credit the entire radiation oncology team for getting me through a very tough time and keeping my spirits up. I never dreaded going to treatment. The radiation and oncology staff would remember me and say ‘hi’ and give me hugs. What a group!”
Her cancer behind her, former schoolteacher Georgia Hartness is enjoying life again.
-

My name is Kelly, and I'm 44 years old, married with three daughters and, as of July, 2014, a new granddaughter. I live in Billings, Montana, and after having a service business for many years, I now provide online technical assistance to people wanting to diagnose and repair their own appliances. I am a ham radio operator and able to incorporate my hobby into my day working from home.
I was diagnosed with an initially unknown type of cancer on December 12, 2014. I was in the hospital in Billings for norovirus, and it was totally by accident that during a scan of my lungs, a tumor was found on my liver. I was quarantined because of the virus, and visitors had to go through a long precautionary process to even enter the room.
Aside from phone calls, the first few days following the news of this tumor were spent isolated from friends and family. That was probably the hardest part, and then the type of tumor couldn't be immediately identified because of its position in my liver. It was hard not to know.
Initially, my wife and a pastor from the hospital did come to offer comfort but were discouraged from returning due to the contagious virus. I was especially concerned about my wife because we had the new granddaughter at home. After a week in the hospital, I was discharged with a referral to Virginia Mason because they were a leading hospital in the type of liver surgery I needed.
I was surprised when I was promptly contacted by the Virginia Mason patient care coordinator with whom I talked at length about what I might expect in the coming weeks. I opted to wait until after Christmas to do anything, so I was able to spend the holiday with my family and the new baby.
Christmas was very special, almost bittersweet, not knowing what the outcome of my cancer might be. When I reached Seattle in early January, I met with several doctors. The course of treatment would include a procedure to see if the tumor was isolated in the liver or if it had spread. There would be lots of scans, blood work and tests.
Fortunately, the tumor did not appear to be outside my liver at all, and I had a portal vein embolization, a procedure to stimulate growth of the healthy part of my liver. With this and every procedure I had, everything was well explained and all my questions answered. I was finally learning what was going on inside of me, and I so appreciated that!
After a very tense month of waiting and a few more tests back home, I was notified that my procedure had been successful and my liver had grown to a size that would allow resection of the tumor … it was go time! On February 5, 2015, I met with the surgeon to go over the operation one last time. He explained, in great detail (with pictures even!), exactly what he would do. I had some very odd questions for him, but he graciously answered every single one of them.
The morning of February 6, I was prepped for my operation, and we were underway. After a very long surgery (more than nine hours), the tumor was successfully removed, and my recovery process would now begin. Aside from the surgery, of course, the most amazing part of my stay was the extraordinary pain control. My pain was managed with an epidural that was very effective, and I was not kept in a zombie-like state with pain medications.
I soon felt great and was up and walking the day after the surgery! My hospital stay was six days, but I opted to stay in Seattle for a few extra days until my follow-up appointment. Everything looked good.
Since returning home I've had several more tests and scans, just to be sure nothing is hiding anywhere. So far, so good. A couple years of quarterly scans will be in my future, but they are very tolerable.
The people I met while at Virginia Mason were amazing. There were so many involved in my care, I wish I could name them all. I will always be grateful for my extraordinary surgeon, who was not just a good doctor, but also a really great person. I have a great deal of respect and admiration for him and can easily attribute my survival to his skill and dedication to his profession.
The patient care coordinator was also an integral part of this whole process. He was the first person I talked with and was the go-to-guy when I had any questions. I appreciated his efforts to keep me informed and on time to all my appointments!
The nurses and other caregivers were also amazing, and I am so grateful for their care. They went way above and beyond what would be expected and made sure I had everything I needed to be comfortable, the little things that are often overlooked, like lip balm, a fan, etc. One of my caregivers always took a minute to talk to me and made me feel that she cared about me, no matter how busy she was. That meant a lot being so far from home! One of the greatest things about coming through this is being more thankful for the moments you have to spend in each day, enjoying the little things that tend to get overlooked and not spending so much time and energy on the less important things. Sure, there are bad days, but if you look back and think, “Look what I have survived!” it puts things into perspective!
After my diagnosis, I was humbled by the number of people who came forward with words of encouragement, financial gifts, and offerings of support and prayer. I was also saddened by a few who I really thought I could count on who were not interested. I thank God for the miracles, starting with the accidental finding of the tumor, all the way through the oddity of it being entirely encapsulated so that it could be completely removed! My wife, Christina, was a huge part of my recovery, and I'm grateful for the way she stepped up to handle the things that I could not.
I look forward to this being part of my past and not something I need to focus on in the coming years. Each day it gets better, and each day is a little celebration as I am able to get out of bed and live life! I look forward to many more celebrations!
-

A 2016 health scare—a benign adrenal gland tumor that required surgery—prompted 73-year-old Greg Corbin to begin taking better care of himself. The self-described heavy drinker and smoker threw out his vodka and cigarettes without looking back. “I haven’t had a drink or a cigarette since that surgery in 2016,” he said.
Taking care of his health meant getting yearly low-dose CT scans to screen for lung cancer, something Greg had never considered before. To his surprise, the scan was quick, simple and painless. “Lung cancer screening is just about the easiest thing anyone could do,” Greg said. “It’s done in under 15 minutes, and you keep your clothing on. There’s nothing invasive or uncomfortable about it. I could fall asleep during a scan!”
His yearly scans were normal until 2019, when he was diagnosed with stage 1A lung cancer in his left lung. The good news: His cancer had been detected at an early stage and had not spread to any other organs.
Greg met with Virginia Mason Franciscan Health thoracic surgeon Thomas Templin II, MD, FACS to discuss his treatment options. He chose surgery to remove the cancerous tissue from his lung and began planning for the procedure with Dr. Templin. The surgery, which took place at St. Joseph Medical Center in Tacoma on May 7, 2020, removed about a fifth of his lung capacity, Greg said. But the payoff was peace of mind.
Now recovered from surgery, Greg enjoys fishing, farming, and cheering for the Seahawks from his 13-acre property bordering the Deschutes River near Olympia, Washington. “I had inaugural season tickets in 1976, but raising a family kept me too busy to go to many games,” said the retired heating and cooling technician. Thanks to his crucial catch, he hopes to be around for many seasons to come.
Catching cancer early, when it’s easiest to treat, means not waiting for symptoms to show, Greg said. “I had no indication of any health problems, and I felt fine. I never would have known I had cancer, and I never would have had the screening if it wasn’t offered to me.”
“If you’ve ever smoked, lung cancer screening is just the right thing to do,” he added. But even those who never smoked can request a scan. “Recently, I lost a childhood friend to stage 4 lung cancer. She didn’t smoke, so she didn’t think she needed to get tested. But what a difference if she would have gotten a CT scan.”
-
Successfully navigating health challenges takes a team. Just ask Mike Gates of Renton, who beat lung cancer in 2019. Confronting cancer meant partnering with his health care team and actively participating in the process, he said. “Don’t rely on others to follow up. It’s your body; it’s your job.”
When Mike began noticing chest pain and shortness of breath a few years ago, he quickly reached out to his primary care provider Juliet Bliss, DO. “I’m pretty proactive about my health, so I asked my family doctor if she could order blood tests and a lung X-ray. The X-ray showed some shadowing in my lung, so I was referred to a pulmonologist, who then ordered a CAT scan.”
The dark shadow turned out to be a suspicious growth in his lung, but it didn’t require treatment just yet. Instead, his care team recommended yearly scans to monitor its growth. In 2019, Mike’s annual screening revealed that the growth had darkened, and additional tests confirmed a diagnosis of early-stage lung cancer.
Mike’s care team, including Virginia Mason Franciscan Health pulmonologist Frederick D Troncales, MD, and thoracic surgeon Baiya Krishnadasan, MD, mapped out a treatment plan to restore Mike’s health. In July 2019, Dr. Krishnadasan performed surgery to remove the cancerous lung tissue.
Now cancer-free, Mike wants others to know that cancer screening isn’t something to fear. “The doctors are professionals, and they’re committed to discovering these things early so they can treat them. It's not that hard to do your part,” he said. “Just follow the steps: When you get your physical, if you feel any issues, ask for some tests. Your doctor will be happy to do it. You can also ask if you’re a candidate for screening based on your age or your health profile.”
The avid Seahawks fan credits his crucial catch to a proactive approach, backed by an expert team of physicians. “I believe I was lucky,” he continued. “I could have waited to get checked, and people do get busy in life … but your health is your wealth. I’ve got nine grandkids, four adult children, and a wife I’ve been with since 1975. It’s just a relief for all the people I love who rely on me.”
-

Rebecca had her yearly physical exam with her PA (Bella Arshinova, PAC) at Franciscan Medical Clinic in Des Moines. During the exam, she went over her health record and reviewed a CT scan of her abdomen that was done a few months back by another physician. In the CT scan, one of the results showed there was a cystic lesion on the border of the heart. Her PA referred her to have an MRI and was diagnosed with a pericardial cyst. Her PA was concerned this could possibly put pressure on the heart if it became larger.
Rebecca was referred to Franciscan Cardiothoracic Surgical Associates in Tacoma and was seen by Thomas Templin, II, MD, FACS. After another CT scan of her chest for the pericardial cyst, the results identified a spot on her lung, which was confirmed as early lung cancer after additional testing.
She was completely shocked by this accidental finding with no idea this diagnosis was even possible given her age and lifestyle, but Dr. Templin was very reassuring, very confident and organized. “He told me, ‘We’re going to take good care of you.’” And that’s exactly what they did. He provided her with all her necessary appointments before she even left the office, so she knew exactly what was going to happen and exactly what to do. She was scheduled for surgery at St. Joseph Medical Center and had 10% of the upper left lobe removed. No radiation and no chemotherapy were needed.
Recovery has been amazing. With the love and support of her son, her brother and sister-in-law from California, and her boyfriend, it helped her relax, rest and heal faster.
-

My name is Matthew. I'm a city manager, and I live in Ellensburg, Washington, with my wife and two children. We love doing outdoor things like camping and bike riding and treasure our annual trip to Disneyland. We are all proper Disney nerds!
Two years ago, I found out I had cancer the day before leaving on our annual Disney trip. While lathering my neck for an old-fashioned razor shave, my barber noticed a big rock-hard lump. While she froze in terror, I immediately realized it was probably cancer and would explain the mysterious symptoms I'd been experiencing.
On Valentine's Day, 2013, a diagnosis of Hodgkin's lymphoma was confirmed. I was confused, but not scared at first. I remember thinking that getting treatment as soon as possible would be beneficial.
The first oncologist we visited was not at Virginia Mason and it was an awful experience. His office was dark and bleak. He sat me down and, without talking to me at all, began detailing a litany of procedures, exams and the like that I would need. When my wife and I left, we were scared and felt very alone.
I went to work the next day in a daze. A friend came by who had heard about my diagnosis and recommended I go to Virginia Mason for treatment. I called right away and found out I could be seen that weekend. It was an answer to my prayers.
From the start, I knew I was in the right place. I had done research before my appointment and found out how good the program was and that I would be seeing one of the top oncologists in the Pacific Northwest. He walked in and his first words were that while I had cancer, and we would treat that, he wanted to know about me as a person and human being. He asked about my hopes, my fears, whether I planned to have more kids, and how chemotherapy might impact that.
He also went over a much smaller list of tests, letting me know that in his opinion the tests the other oncologist wanted (such as a bone marrow biopsy) were most likely not needed. He explained the benefits of a “port” over other infusion methods, and I left hopeful and confident we would beat Hodgkin’s!
My cancer treatment was “surreal” in a good way. Virginia Mason has gone to great lengths to make the experience as comfortable and stress-free as possible. I had several chemotherapy regimens and a stem cell transplant. It was a huge and unique benefit that all my care was provided in the same facility and test results were always returned the same day. I never had to “go home and wait.” As anyone who has faced cancer knows, a long wait for test results is just dreadful!
Everyone we met—from the janitors to the volunteer concierge cart folks to people in radiology, general surgery and all throughout the organization—had passionately embraced a culture of service, positivity, safety and professionalism. We had a seemingly tireless team of health care professionals who fought the good fight with us, comforted us, and helped us heal both emotionally and physically.
My daughter has severe anxiety disorder, so you might imagine what my diagnosis and treatment did to her. Virginia Mason staff went out of their way to include her where appropriate, empower her to help, and to understand the process. I could go on for quite some time bragging about so many amazing people at Virginia Mason!
All that said, it wasn't an easy road. I remember just after one of my chemotherapy treatments that my kids woke me up one day and said, "Dad, we are so sorry to bother you, we know you're sick, but can you please make us some breakfast? We don't know how." That broke my heart. My sweet kids, so compassionate and needing something so simple that was almost impossible for me to do.
This experience has taught me so much about the journey of life we are all on. I find myself wanting to give back, to comfort and help others as they face a cancer diagnosis. People tell me I am way more relaxed and “laid-back.” Having faced the shadow of death helps you figure out what's truly important.
I think I am in a “new normal.” I am considered cancer-free, but I don’t want to forget the experience that has gotten me to this point. Today, I am grateful for everything and take nothing for granted, not one single moment.
-

I noticed a tiny bump on my right shoulder blade. I’m very conscientious of my body, and when I saw a change, I had it checked out right away. My doctor removed the bump and sent it to a lab. It was melanoma. I had surgery to remove the tumor, which was about five inches deep into the muscle. Since the cancer was so unusual, I had a full body MRI and brain scan. The MRI showed stage 4 cancer in my right lung, so surgeons removed that tumor. Today, I’m cancer-free.
-

My name is Kris, and I'm happy to say I turned 63 in April 2015. When I was diagnosed with pancreatic cancer on Jan. 6, 2011, it was a very, very dark day. At that time, I had a teenage son and daughter, two bichon frises, a bunny, and a wonderful husband I’d been with for 27 years.
I also had two aunts who had died of pancreatic cancer, one I was particularly close to. I remember very clearly when my primary care physician called to tell me the results of a CAT scan she had ordered. I told her, “Don’t tell me this! This is a death sentence!” I was horrified.
I immediately contacted my sister, a trauma surgeon at Cook County Hospital in Chicago. They say that the Lord works in mysterious ways. At that time, my sister was studying for another board certification. She had just read a paper written by a Virginia Mason oncologist about the team approach to treating pancreatic cancer.
She asked if I was aware of Virginia Mason and I responded that I had been getting my care there for more than 20 years! She urged me to talk with the physician who had written the article she had read because "he totally gets it”—that cancer has to be looked at holistically. His protocol and the Virginia Mason approach, she said, appeared to be quite unique in the treatment of pancreatic cancer.
I met this oncologist for the first time in a joint meeting with my surgeon. I loved him right away. He has twinkly eyes; a very honest, straightforward manner; and a sense of humor. That trust was confirmed when he came into my hospital room at 9:30 at night, the day after my surgery. The diagnosis of stage 2 pancreatic cancer had just been confirmed, and my husband and I were both having a good cry.
This doctor introduced himself again and then sat down on the foot of my bed. He said, "What information can I give you that will help you sleep tonight?” He then proceeded to patiently answer our zillion questions. But the answer that meant most to me was when my husband asked him, “What do you consider to be your role in this proposed treatment?” He answered, “My role is to be Kris’ spiritual cheerleader. Anyone can write a script for chemotherapy. But if I can help keep her spirit strong, she will win.”
He proceeded to talk about how cancer was perceived to be a battle waged by the human body. But it was also a battle being waged by the human spirit. I knew I had found the right doctor. Oh, I checked out the competition—but it wasn’t even close.
It is still difficult to talk about the one year of adjuvant therapy. I was very sick, and the physical toll it took was a mighty one. But I had the best team in the world. All the oncology nurses were the most compassionate, lovely people. They always gave me a boost, helped me to laugh, and worked so hard to alleviate the terrible side effects. This started even before I got to the treatment room, with the wonderful ladies at the front desk on the second floor who checked me in.
But as awful as 2011 was, it was also a year of many blessings. I developed an extraordinarily close relationship with my daughter. I learned to be a gracious recipient of help. I tell my children and everyone who asks that my survival was not due to some special effort from me.
Rather, it was the prayers, compassion and kindness of a village. From the neighbors who snuck in at night to fill my garden with tulip bulbs, to the “soccer moms” who brought dinner to my family, every night, for months in a row, to my two best friends, who sat with me every day for an entire year, and to my Virginia Mason “team”—I am here because of you.
I saw my daughter graduate and head off to college. I taught my son how to drive (now there is a challenge!). I went back to work full time—something even the Social Security office had a hard time believing. My life has been changed irrevocably. I laugh more. I spend more time with the people I love. My faith has deepened.
I truly believe that Virginia Mason gave me the means to live a full and complete life. Having such a serious illness leaves a shadow. It is always there, flitting around the edges. I don’t dwell on it. I’ve been very fortunate to be invited to work with Virginia Mason to improve the patient experience, through workshops and participating in process improvement sessions.
The dedication I see from the Virginia Mason team is an inspiration. Life after cancer is not “normal.” It’s better than that. Continuing my relationship with Virginia Mason is part of that “better.” Whatever I can do to give back is such a small price to pay for the amazing care I received and continue to receive. Thank you, thank you. As my son would say, “You totally rock!”
-

Ky Hopewell was facing a daunting surgery to remove a potentially malignant cyst from his pancreas. A long-time Federal Way resident, his South Sound physician told him he was a candidate for the Whipple procedure, where the duodenum and sections of the pancreas, stomach, small intestine, gall bladder and common bile ducts would be removed. The remaining section of pancreas and small intestine would then be rerouted to a new opening in the stomach and the remaining bile duct reconnected to the small intestine.
Ky, and his wife, Mary Ann, knew he was in for a long recovery.
Thankfully, before Ky went ahead with the procedure, he followed a neighbor's recommendation that he get a second opinion from Virginia Mason surgeon Scott Helton, MD. Dr. Helton, the director of Virginia Mason’s Liver, Pancreas and Biliary Surgical Center of Excellence, and the team of surgeons at Virginia Mason, perform substantially more Whipple procedures than any medical center in Washington state. Studies show that hospitals that perform a high number of the procedures have higher success rates. So Ky already knew he was in good hands.
When Dr. Helton began surgery, he performed an intraoperative ultrasound and noted that the cyst, which was 1.3 inches in length, was benign and only a quarter of it was encapsulated by the pancreas. This presented a new option, to enucleate or shell out the tumor. He had executed this procedure on other tumors, but never on this type of cyst. Although there were challenges with this method, such as GI bleeding, this method appealed to Dr. Helton in that, unlike the Whipple, it allowed more preservation of Ky's healthy organs.
Thankfully, Ky didn't experience any pancreatic leakage or GI bleeding. Instead of being in the hospital 14 days, Ky went home after five days. And his predicted two-month home recovery dropped to eight days. “I feel great. I'm back at work and able to keep up with the activities I did before I was diagnosed.” These include keeping up with two grandchildren and volunteering for Reach Out Federal Way, a program that benefits homeless men and women.
Ky adds with a smile, “Getting the second opinion from Dr. Helton was the best decision I made.”
-

I’m 58 years old and was recovering from major surgery last year when I learned I had peritoneal cancer, which affects a thin layer of tissue that lines the abdomen. At first, I was in shock. When that wore off, I wanted to know what the next step was and what the treatment plan would be.
I never considered getting my treatment anywhere other than Virginia Mason. My gynecologist of 20 years practices there, and I trust her completely. She referred me to another Virginia Mason gynecologist who is a cancer specialist. Together, they created a treatment plan and discussed it with me at length. All my questions were answered, and I was comfortable with the plan.
Nothing, however, could have prepared me for how grueling cancer treatments can be. Every week for three and a half months, I came to Virginia Mason for chemotherapy. And while I didn’t look forward to the treatments, which caused me to lose my hair and 30 pounds, I did enjoy seeing the people who cared for me. They became like friends, and one of my nurses was with me every single step of the way through the entire treatments. She went out of her way to make sure I was always comfortable, and I knew I could ask her anything.
I am now considered a cancer “survivor” and feel fortunate that I had the best care possible. And I had so much support from my husband, family and friends.
Through this experience, when just getting out of bed might take every ounce of energy, I've learned that I'm stronger than I ever thought I was. Sometimes, I had to convince myself to stay positive, and I managed to do that more often than not.
Today, I appreciate things more and complain less. I spend time gardening, and I work two days a week as I prepare for retirement. I feel lucky that I received my care at Virginia Mason. I can't imagine a better place to be.
-
My name is Bill, and I am a software engineer. In fall 2010, I was sitting on my father's front porch in Milwaukee when I got the call confirming I had prostate cancer, the same disease that had killed my grandfather and was about to end my father's life as well.
Because of my family history, for years I had regular prostate-specific antigen (PSA) tests. The PSA level is often elevated in men with prostate cancer, and in the years just prior to 2010, my numbers were going up. Some doctors adopt a “watch and wait” approach to rising PSA levels when there are no symptoms. But my doctor recommended I see a urologist who specializes in diagnosing and treating prostate cancer. I'm glad he did.
The urologist recommended a new gene-based test called a PCA3, and the results were “positive,” meaning there was a strong likelihood I had prostate cancer. A biopsy was needed for confirmation, and during that operation, 17 samples of prostate tissue were removed. Three were found to contain cancer cells. The good news was that my cancer was detected early and confined to one part of my prostate. This meant that with proper treatment, my prognosis was excellent.
Chemotherapy, radiation and surgery are all used to treat prostate cancer. After researching my options, I chose to have surgery at Virginia Mason because, as I learned, it's one of the best places in the country for this type of operation. After I decided on Virginia Mason, I was also accepted into the clinical trial of a new treatment being tested as an adjunct to surgery. In the weeks prior to my operation, I visited Virginia Mason frequently as part of this clinical trial. With every visit, I felt more certain I was in the best possible hands.
On the day of the surgery, everything went smoothly. My hospital stay and follow-up care were first-rate. I actually returned to work after only three days off.
Today, I am considered cancer-free. I am back to enjoying hiking, biking and kayaking. And while I continue to be monitored closely, my focus is not on cancer but on the people I love: my wife and five children/stepchildren.
My life has changed in positive ways. I have more gratitude, more awareness that I want to enjoy the life God has given me, and more urgency to do things today, not tomorrow. I'm grateful for the care I received at Virginia Mason. And to the people who provided that great care, I send my heartfelt thanks.
-

It’s common for prostate cancer to progress without any symptoms. This makes the disease more likely to advance before you know something is wrong. Fortunately, the PSA blood test is a screening tool that can lead to early detection and treatment.
Christopher S. Arroyo, MD, a urologist and surgeon at Franciscan Urology Associates in Gig Harbor, recommends prostate screenings for men who are at risk for the disease. This includes those over age 50, men who have a family history of the disease, or those who are of African American ancestry who have at least a 10-year life expectancy.
Weighing the options
Port Orchard resident Bill Szpor learned his PSA levels were high as a result of a prostate screening by his general practitioner. He was referred to Dr. Arroyo.
“Dr. Arroyo spent time with my wife and me, and he talked to us about everything,” Bill said. “He told us to take a few days and then come back and tell him what we wanted to do. My wife and I sat down and weighed the options. I had an enlarged prostate and a little bit of cancer in the prostate. We believed the best way to deal with it was to eliminate the problem. We weighed the downsides against the positives and decided to just take it out.” Dr. Arroyo performed the procedure—a robotic prostatectomy.
Informed decisions
Prostate cancer diagnosis and treatment is a very controversial topic, said Dr. Arroyo. “The reason is that many prostate cancers are small-volume, slow-growing cancers, and they tend to occur in older men—so for some men, the cancer may not be life-threatening. One of the first things I do with patients is to put their cancer in context of their health condition, their age, and their level of comfort with ‘sitting on’ the cancer if it isn’t life-threatening.”
When individuals are candidates for curative treatment, meaning they have an early cancer that has not spread outside the prostate but has the potential to become life-threatening, the discussion advances to exploring treatment options, recovery and the potential complications, he said.
Compassionate care
There is a lot of information to process and decisions to be made after a cancer diagnosis. The experts at Virginia Mason Franciscan Health are here to answer any questions you may have, and to make sure you are informed about all your treatment options. Our team works together to make sure you receive high-quality, compassionate care.
Cancer care is provided by Virginia Mason Franciscan Health and a network of expert partners, including Peninsula Radiation Oncology, Northwest Medical Specialties, TRA Medical Imaging and the Puget Sound Institute of Pathology.
-
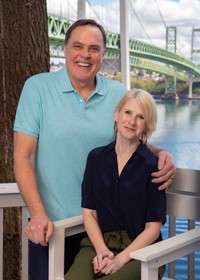
Bob Reemts of Gig Harbor knows all the reasons men put off prostate exams. After he experienced aggressive prostate cancer at age 58, he started encouraging his friends and relatives to get screened and heard the familiar excuses. “Men don’t like the idea of a rectal exam, and they’re scared of the treatment if they do have cancer,” he said. “They’re worried about the effects of surgery.”
Bob can relate to those concerns. But when his partner, Jenny, asked him to get his prostate checked in 2015, he obliged, even though he wasn’t experiencing any of the common symptoms of prostate cancer like frequent urination or lower back pain. “Women are often the ones who have to cajole their significant others into getting screened,” he said.
To his surprise, Bob’s exam revealed highly aggressive prostate cancer—caught just in time. Had Bob waited much longer to get screened, his cancer may have spread to his bones, with a much worse outcome, he said. Virginia Mason Franciscan Health providers primary care physician John Smoots, MD, and urologist and surgeon Robert Johnston, MD, Ph.D., developed Bob’s treatment plan together with oncologist Dr. John McCroskey at NW Cancer Specialties.
Bob’s prostate and surrounding tissues were removed in a robotic-assisted, minimally invasive prostatectomy surgery performed by Dr. Johnston at St. Joseph Medical Center in Tacoma. “My care team was excellent, and all three providers collaborated on my treatment plan. Rob and Dr. Johnston especially worked together when I had chemotherapy,” he said. “These connections are why I ended up with such a good outcome.”
Jenny and Bob married in 2016, the day before he began chemotherapy. Her support helped get him through from diagnosis to recovery, he said. Bob encourages men to face their fears and get screened, for themselves and their loved ones. “My family is what got me through this, my boys and my two stepkids and Jenny in particular—she was my rock.”
-
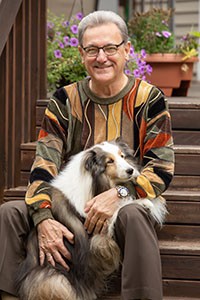
When it comes to prostate cancer screening, 72-year-old Dave Carter doesn’t mince words. “Get a simple little blood test to get your PSA checked. It takes 30 seconds, and it can save your life,” he said.
He’s living proof. In 2017, after his routine prostate-specific antigen (PSA) test came back abnormally high, Carter was referred to Virginia Mason Franciscan Health urologist Manas Jain, MD. After additional testing, Dave was diagnosed with prostate cancer. “People ask me how I knew I had cancer, and I always tell them that I didn’t know. I had no symptoms, everything was functioning, and I felt fine,” he said.
Swift surgical treatment followed, and routine PSA screenings showed no signs of cancer. But Carter, who retired in Port Orchard after a 30-year Naval career, still felt unwell. He scheduled a visit with Dr. Jain in early 2020 and learned that his prostate cancer had spread to surrounding organs.
Carter had little time to adjust to his new diagnosis of stage 4 prostate cancer. Not one to back down from a challenge, he met with Virginia Mason Franciscan Health oncologist Sirisha Jain, MD, and began regular chemotherapy treatment.
In August 2020, Dr. Manus Jain gave Carter the good news: The cancer was nowhere to be found. “My treatment worked better than expected, and I’m now cancer-free,” Carter said.
Routine PSA screenings are vital, because prostate cancer is a silent killer, he said. “Nothing indicated to me that I had a prostate problem … don’t assume that because you’re 27 or 37 or a weightlifter or a marathon runner that it can’t happen to you. I’m passionate about this because I’m trying to save your life.”
-

For men, it’s common for early-stage prostate cancer to progress without symptoms. This makes the disease more likely to advance before you know something is wrong. Fortunately, prostate cancer screenings can lead to earlier detection at a more treatable stage.
The PSA blood test and digital rectal exam (DRE) are two screening tools used to check for red flags that could indicate cancer. If either of these screenings produces suspicious results, the next step is an ultrasound-guided biopsy, said Dean Mastras, MD, radiation oncologist at Tacoma Radiation Oncology. Your age, race and family medical history are some of the factors that determine when you should begin discussing screening options with your doctor. Typically screening begins between ages 40 and 50.
The power of screening
Olympia resident George Madsen can attest to the importance of screening. In December 2013, his doctor found a lump during his annual physical, which included a DRE. A biopsy subsequently revealed prostate cancer. “It was eye-opening,” George said. “It put my own mortality front and center.”
Researching options
The initial step of trying to figure out what comes next after diagnosis is one of the hardest, said Dr. Mastras. In cases where treatment is necessary, every man has choices. But which choice is best for you?
There is a lot of information to consider, and sometimes the abundance of data can be overwhelming, Dr. Mastras acknowledged. For George, researching every option to the extent possible was important, but it became frustrating as he frequently encountered biased information. After traveling to various specialists and reading a lot of research on his own, his pursuit for information led him to Dr. Mastras.
During a three-hour consultation, Dr. Mastras shared well-graphed, long-term data with George that compared research looking at men of similar age and stage and grade of disease. “I try to stay away from biases. Falling back on the data and outcomes is the best way to consult patients,” Dr. Mastras said. George appreciated his approach. His concerns about side effects and the possibility that the cancer would return after his treatment ended were addressed by Dr. Mastras in a factual, compassionate manner.
“Dr. Mastras comes across as very human, very down-to-earth, and has a great sense of humor. I appreciate that. It is already a tough enough situation coming to grips with the ‘C’ word,” said George. “Dr. Mastras put me at ease.”
Cancer care is provided by Virginia Mason Franciscan Health and a network of expert partners, including Tacoma Radiation Oncology, Virginia Mason, Northwest Medical Specialties, TRA Medical Imaging and the Puget Sound Institute of Pathology
-

Could you have cancer and not know it? For men, it’s common for prostate cancer to progress without any symptoms. This makes the disease more likely to advance before you know something is wrong. Fortunately, there is the PSA blood test, a screening tool that can lead to early diagnosis and treatment.
When Leo Hastings of Libby, Montana, received his prostate cancer diagnosis, he traveled to Tacoma for treatment led by Dr. Johnston. Leo’s son was familiar with Virginia Mason Franciscan Health and wanted his dad to have the best care—and to him, that meant Dr. Johnston and the staff at Franciscan Urology Associates in Tacoma.
Feeling at ease
Navigating the process of choosing a treatment team can be daunting. Finding the right team can be a relief. “After I met Dr. Johnston, I felt confident I was in good hands,” said Leo. “He seemed to know and understand what he was talking about, and he didn’t talk around corners. He laid it out to you—I liked that. He was very knowledgeable and educated.”
Dr. Johnston explored treatment options with Leo and helped him feel at ease with his decision. “Depending on the stage of disease, prostate cancer may be treated in several ways. On many levels it is a matter of personal preference,” said Dr. Johnston.
Some prostate cancers progress so slowly that no immediate treatment is required. In such instances, “active surveillance” may be warranted, meaning periodic blood tests and rectal exams are used to monitor disease progress. If the cancer is advanced or growing, other options such as radiation, hormone therapy, chemotherapy, immunotherapy or surgery may be considered. It is a very individual decision in which a person must weigh the potential outcome with the risk of side effects and impact on their preferred lifestyle.
Compassionate care
There is a lot of information to process and decisions to be made after a cancer diagnosis. The experts at Virginia Mason Franciscan Health are here to answer any questions you may have and make sure you are informed about all your treatment options. Our team works together to make sure you receive high-quality, compassionate care.
Cancer care is provided by Virginia Mason Franciscan Health and a network of expert partners, including Tacoma Radiation Oncology, Virginia Mason, Northwest Medical Specialties, TRA Medical Imaging and the Puget Sound Institute of Pathology.
-

It’s common for testicular cancer to progress without any symptoms, making the disease more likely to advance before you know something is wrong. Most often testicular cancer occurs in men ages of 20 to 34, but infants and elderly men can also develop this disease.
When Seattle resident Kevin Roundtree learned he might have cancer, he turned to Highline Cancer Center for answers.
Just that fast
One moment Kevin was finishing up at work, and the next he was rushing himself to the hospital. The swelling he experienced made it obvious something was wrong. The doctor said it might be a blockage or it could be testicular cancer. At 47 years old and in good health, Kevin was stunned. “I’m kind of a rough and tumble, busted up, been sewn up more than a pair of Levi’s kind of guy, and this one caught me by surprise.”
Finding your way
“What it comes down to, what’s really most important, isn’t my ego or my emotions; it’s my family. I’ve got three kids and a wife. I wasn’t ready to die. You really have to get fit with your emotions, figure out which way you’re gonna go, and then hit it.” Kevin didn’t want to waste time. He and his wife, Jodie, went to see a medical oncologist at Franciscan Oncology Associates in Burien, part of the Highline Cancer Care team.
Kevin was willing to do whatever it would take to get the cancer out of his body. The doctor explored the options with him, and they came up with a treatment plan. Kevin has nothing but praise for the doctor and nurses at Highline, who he says won the fight for him. “The nurses at the cancer center allowed me to function my way to get better,” he said. “I didn’t want to lie down and be sick. I needed to keep moving, keep working and keep living. They helped me to do that.”
Life after treatment
Now that chemotherapy is finished, Kevin still remains vigilant. He will continue seeing his doctor for regular follow-ups so they can monitor his health and watch for relapse. “Follow-up appointments are essential,” said the doctor. “We not only monitor for signs of the cancer returning; we also watch for treatment side effects. Blood tests and imaging tests such as X-rays or CT scans can help us detect relapse at an early stage.”
-
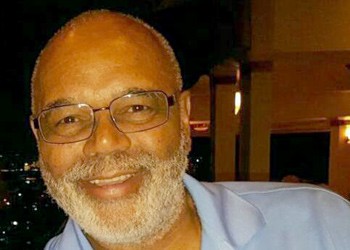
My name is Ron. I'm 68, a retired Washington state patrolman, and I own a driving school with my wife, Linda, our son and daughter-in-law. I've always been someone who is cautious about my health, and that's why it was a shock to learn I had prostate cancer. Except for high blood pressure, I've been pretty healthy all my life.
My first urologist dealing with the prostate cancer diagnosis was not at Virginia Mason. I'm sure he was a fine doctor, but he wasn't the one for me. A friend who had been treated at Virginia Mason said he was impressed with his doctor there, so my wife made an appointment for me.
From the minute I met the Virginia Mason urologist, I liked and trusted him. He was very honest about what prostate cancer means and about the different kinds of treatments available. The other thing I liked about that appointment was that we didn't feel rushed. The doctor answered every question we had. This was on a Thursday, and he scheduled a CT scan for the following Monday.
It saved my life because while it was supposed to be a routine look at the cancer, the CT scan revealed I had an aortic abdominal aneurysm. This is an enlarged area in the main vessel that supplies blood to the body from the heart. If this aneurysm had ruptured, it could have killed me in minutes. Often, as was the case with me, there are no symptoms.
My urologist and his team quickly scheduled me for a consult with a Virginia Mason vascular surgeon who set surgery for the following week. On that Thursday, however, I became faint, and my blood pressure had escalated to extremely unsafe levels. I went to a local ER where they insisted I have surgery for the aneurysm there. I was adamant that I be treated by my vascular surgeon. The ER doctor would not allow this until he spoke to my doctor at Virginia Mason. After several phone calls this was accomplished, and I was transported to Virginia Mason via ambulance. Within an hour after arriving, both the vascular surgeon and urologist came to my room to talk to me about what needed to be done. The surgeon performed a successful operation on the aneurysm early the next morning, and I was soon able to go home.
Meanwhile, I was still vacillating about whether to treat my prostate cancer with surgery or chemotherapy and radiation. I took a short vacation with my family, and when I returned, I decided to have the surgery. Again, it was a success. I've had a few issues with my bladder that are slowly improving, and I will be doing follow-up radiology as a precaution.
Through all of this, the thing that has really impressed me about Virginia Mason is that there are no "unknowns." Every question gets answered, and I've never felt confused or worried. Everyone always has the time to talk with me at every level. From the moment you walk in the door to the moment you leave, you feel like the focus is on you. When you're dealing with a serious medical issue like cancer, it can't get much better than that.
-

When Dan Dahl was diagnosed with trachea cancer, he looked at his two sons, then ages 6 and 9, and determined, “I've got to stay alive to raise these boys.”
He had just turned 40 when shortness of breath and bouts of coughing sent him to a pulmonologist at Virginia Mason. After a number of tests, a tumor was found on his trachea. The tumor was not malignant at the time, and over the next six months, Dan underwent laser therapy in an attempt to vaporize it. But the tumor was aggressive. Not only did it grow back on both sides of his trachea; it also turned into squamous cell carcinoma.
While other types of cancer can spread to the trachea (also called the windpipe), cancer that originates in the trachea is very rare, accounting for less than 0.4 percent of all cancers. Tracheal tumors are often difficult to diagnose because they are slow growing and don't always show up on initial imaging.
Squamous cell carcinoma is usually associated with smoking, but Dan had never smoked. Instead, he was young and fit, an avid skier and hiker who had climbed Mount Rainier a few years before.
Because the blood supply to the trachea is so delicate, surgery to remove a tumor in the windpipe can be quite complex. In Dan's case, surgeons at Virginia Mason removed one of his ribs to gain access to his trachea. After surgery, he underwent three months of radiation therapy.
And that was it. Two years after cancer treatment, he conquered Mount Rainer again in a celebration of life. Now, more than 27 years after treatment, he's had no recurrence of cancer.
But he has had other conditions that brought him back to Virginia Mason. At 57, cardiologists discovered a blockage of the left main artery of his heart, which required bypass surgery. In harvesting a vein in his leg to be used for the bypass, doctors were able to use endoscopes and small incisions—instead of the traditional open surgery—to retrieve the vein. This made a huge difference in Dan's recovery, and he was soon back to taking his 5-mile walks.
Then, a few years ago, Dan came back to Virginia Mason for repair of a hiatal hernia that was so massive it was pressing his stomach up into the chest cavity, making it difficult to breath. Thoracic surgeons did the repair, which dramatically improved his lung capacity.
Through it all, Dan never missed a ski season. Today, at 67, he and his wife, Sandy, spend winters in Sun Valley, Idaho, and ski about 60 times a year. Both are grateful to Virginia Mason for helping them live a full life together.
“I owe my life to Virginia Mason,” he said. “I feel like I can get great doctors and great care for just about anything.”
And those two little boys Dan was so determined to raise? They grew up to be fine young men. And now, with grandchildren ages 4 and 9, Dan is enjoying watching the next generation grow up as well.