Brain Tumor Treatment
Virginia Mason Franciscan Health's Brain Tumor Program offers a team of surgeons and physicians who specialize in brain tumors. The care of patients with brain tumors is complex and differs from tumors or cancers in other parts of the body. Patients with brain tumors have unique symptoms and neurologic complications that require specialized care. We treat all brain tumors ranging from benign to malignant. For spine tumors, see our outstanding spine team.
Neuro-oncology services
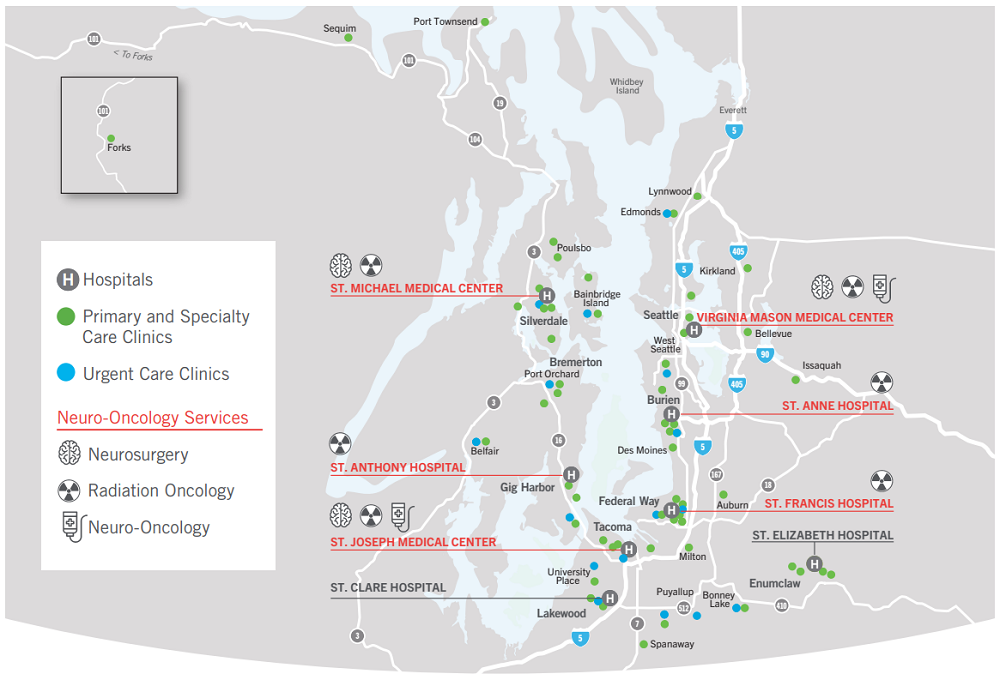
Virginia Mason Franciscan Health's Brain Tumor Program offers world-class care that is convenient for you. Our commitment is to deliver the best possible care while minimizing the burden on our patients. See the map below which summarizes where treatment is available near you. We also offer telemedicine to allow you to speak with a physician from your home.
Our team
Treatment of brain tumors and brain cancers is performed by a team of highly specialized physicians. The team may vary depending on the type of tumor or its location, but usually will consist of a neurosurgeon, a radiation oncologist, and a neuro-oncologist or medical oncologist.
-
Dedicated tumor and cranial neurosurgeons perform a high volume of complex surgeries each year. We offer neurosurgery at Virginia Mason Medical Center in Seattle, St. Joseph Medical Center in Tacoma, and St. Michael Medical Center in Silverdale.
-
Radiation oncologists are specialized doctors who use advanced techniques to treat brain tumors and brain cancers using focused radiation that damages tumor DNA. Radiation therapy can be delivered at Virginia Mason Medical Center in Seattle, St. Francis Hospital in Federal Way, St. Joseph Medical Center in Tacoma, St. Michael Medical Center in Silverdale, Jane Thompson Russell Cancer Center at St. Anthony Hospital in Gig Harbor, and St. Anne Cancer Center in Burien.
Tacoma Valley Radiation Oncology Partnership
What we offer
We offer all standard of care therapies including diagnostic imaging, neurosurgery (including awake language and motor mapping, fluorescent tumor dye, and other advanced surgical techniques) radiation therapy, stereotactic radiosurgery (Gamma Knife), Tumor Treating Fields, chemotherapy, immunotherapies, targeted molecular therapies, advanced imaging modalities, and advanced molecular testing. We treat any and all types of brain and spine tumors and cancers, including metastatic disease. New or complex cases are reviewed in a multidisciplinary tumor board that includes neurosurgeons, radiation oncologists, neuroradiologists, pathologists, neuro-oncologists, and/or medical oncologists.
GammaTile
Virginia Mason Franciscan Health is the only system that offers GammaTile in the Pacific Northwest, currently available in Seattle and Tacoma. This is a new technology that allows for intraoperative radiation treatment. At the time of surgery, the surgeon places “tiles” that contain a short-lived radiation source in the cavity where the tumor was removed from. This means that treatment of any remaining tumor cells starts immediately rather than waiting for weeks after surgery until standard radiation can begin. Additionally, it may mean that the patient does not need to do subsequent radiation treatment. This is especially useful to reduce toxicity to surrounding brain tissue when treating recurrent brain tumors which have already received external beam radiation therapy.
Clinical trials
New treatments are tested first in animals and then move to clinical trials if the initial data is promising. Clinical trials come in 3 phases:
- Phase 1 studies test the safety and appropriate dose of the drug in humans
- Phase 2 studies confirm safety and also give an initial indication of whether the drug is effective
- Phase 3 studies are large studies intended to confirm benefit from a drug with a goal of changing the standard of care
At Virginia Mason Franciscan Health, we are committed to offering our patients access to advanced therapies in a safe, accessible way. We select clinical trials that have a good safety profile and strong data behind them, and we aim to offer them in multiple locations to minimize the burden of participation. We have multiple open clinical trials but we recommend discussing this with your neuro-oncologist, as it can be difficult to navigate the requirements for each trial.
Brain tumor clinical trial information
-
BN011: A Phase III Trial of Lomustine-Temozolomide Combination Therapy Versus Standard Temozolomide in Patients with Methylated MGMT Promoter Glioblastoma.
MGMT gene “methylation” refers to an alteration that reduces or prevents expression of the MGMT enzyme. This enzyme is able to specifically correct the DNA damage inflicted on the tumor by chemotherapy (temozolomide). Tumors with MGMT methylation are therefore more sensitive to the effects of temozolomide, because they lack the protective enzyme. The rationale behind this trial is to try to target this vulnerability by adding a second chemotherapy to temozolomide. A small European phase 3 trial tested this strategy and found improved survival in patients treated with dual chemotherapies, compared to those treated with standard of care using one chemotherapy. The current trial is attempting to confirm this effect with a goal of changing the standard of care for MGMT methylated glioblastoma in the United States.
- Treatment study: yes
- Randomized: yes
- Currently enrolling: yes
- Optune: not allowed
- Locations: Virginia Mason (downtown Seattle) and Virginia Mason Federal Way
BN007: A Randomized Phase II/III Open-Label Study of Ipilimumab and Nivolumab Versus Temozolomide In Patients With Newly Diagnosed MGMT (Tumor O-6-Methylguanine DNA Methyltransferase) Unmethylated Glioblastoma
For tumors without MGMT methylation, we offer a trial using immunotherapy to entice the immune system to attack the tumor. One of the functions of the immune system is to look for abnormal cells like cancer cells, and destroy them. In response, cancers develop “off” signals that deactivate nearby immune cells. “Immunotherapy” drugs like ipilimumab (Yervoy) and nivolumab (Opdivo) block these off signals, and allow the immune system access to the tumor. In this trial, patients receive either standard treatment with radiation and chemotherapy (temozolomide), or they receive radiation followed by immunotherapy. The trial is currently a phase 3 trial, which means that the goal of the trial is to change standard of care for MGMT unmethylated glioblastoma.
- Treatment study: yes
- Randomized: yes
- Currently enrolling: no - paused for a planned analysis
- Optune: not allowed
- Locations: Virginia Mason (downtown Seattle) and Virginia Mason Federal Way
-
GammaTile START Registry
For selected patients with recurrent glioblastoma, we offer a novel technology that combines surgery to remove the recurrent tumor, with implantation of “tiles” that contain a short-lived radiation source and emit radiation for several centimeters from the edge of the resection cavity, where they are placed at the end of surgery. This remains an experimental strategy, and we are participating in a registry to track the outcomes for patients treated with GammaTile.
- Treatment study: yes
- Randomized: no - all patients are treated with resection and GammaTile
- Currently enrolling: yes
- Optune: allowed
- Locations: Virginia Mason (downtown Seattle) and St. Joseph Medical Center (Tacoma)
Patient Reported Symptom Review (PaRSR)
This is a trial that tracks patients’ predicted symptoms over time and attempts to better understand if subtle changes in symptoms portend tumor regrowth. Each part of the brain has a specific function, and therefore the location of a brain tumor determines the symptoms experienced by the patient. Glioblastomas recur in the original location about 85% of the time, therefore a patient’s symptoms at recurrence should be predictable. Patients fill out a brief email survey every 2 weeks tracking their symptoms, and their answers are correlated to their MRIs and clinical course.
- Treatment study: no
- Randomized: no
- Currently enrolling: yes
- Optune: allowed
- Locations: Virginia Mason (downtown Seattle) and St. Joseph Medical Center (Tacoma)
Resources for patients
-
Brain cancer is the growth of abnormal cells in the brain or skull. A brain tumor may be either cancerous (malignant) or noncancerous (benign). Both types of tumors are serious because either one can compress and damage brain tissue. Both can also cause identical symptoms.
Brain cancer is either a primary cancer, meaning that it originates within the brain, or is a secondary cancer, meaning that it has spread (metastasized) to the brain from another site in the body, such as a lung or breast. When tumors from the body spread to the brain, they contain cancer cells from the original tumor.
A cancer that originates in the brain rarely spreads to other parts of the body, but it may spread to other parts of the brain or spinal cord.
Common brain tumors include:
- Glioblastoma
- Oligodendroglioma
- Choroid plexus tumors
- Pituitary adenoma
- Pilocytic astrocytoma
- Meningioma
- Ependymoma
- DNET
- Craniopharyngioma
- Astrocytoma
- Medulloblastoma
- Pineal tumors
- Vestibular schwannoma
-
Even a small tumor can cause symptoms, such as headaches, seizures or bleeding. Most tumors, however, cause no symptoms until they have grown large enough to compress brain tissue, which can then also cause any of the following:
- Personality change
- Weakness or paralysis in an arm or leg
- Drowsiness
- Difficulty seeing
- Nausea
- Numbness on one side of the body
- Difficulty speaking
- Vomiting
- Confusion
- Difficulty swallowing
It is important to understand that ultimately the symptoms caused by a tumor are dependent primarily on the location of the tumor, and the natural function of the brain in this location.
-
Treatment for a brain tumor is determined based on the type, size and location of the tumor, as well as the patient's overall health. Surgery is frequently performed to remove all or as much of the tumor as possible. In some cases, tumors can be completely cured with only surgery, without the need for further treatment. Advances in radiation therapy, chemotherapy and medications can also contribute to effective treatment and the control of symptoms.
We offer all standard of care therapies including diagnostic imaging, neurosurgery (including awake language and motor mapping, fluorescent tumor dye, LITT—laser interstitial thermal therapy, and other advanced surgical techniques) radiation therapy, stereotactic radiosurgery (Gamma Knife), Tumor Treating Fields, chemotherapy, immunotherapies, targeted molecular therapies, advanced imaging modalities, and advanced molecular testing. We treat any and all types of brain and spine tumors and cancers, including metastatic disease. New or complex cases are reviewed in a multidisciplinary tumor board that includes neurosurgeons, radiation oncologists, neuroradiologists, pathologists, neuro-oncologists, and/or medical oncologists.
-
Radiation therapy uses high-energy beams aimed at the tumor site to kill cancer cells. The beams are delivered in specialized machines that deliver radiation from multiple directions so that they converge at the desired location, to maximize the ability to treat the tumor or cancer and minimize the effect on normal tissue. Doctors who administer radiation therapy are called radiation oncologists. Types of radiation therapy include:
- External beam radiation: This form of radiation therapy delivers radiation specifically to the area of the brain where the tumor is located, or it can be applied to the whole brain. A course of therapy often lasts five to six weeks.
- Stereotactic radiosurgery: Radiosurgery can be an option when a brain tumor cannot be removed with traditional surgery. Stereotactic radiosurgery uses multiple beams of radiation precisely focused on the tumor. A stereotactic radiosurgery course is typically 1-5 treatments every day or every other day. Using computer-generated 3D images of the brain to target the beams, high doses of radiation are delivered to the tumor with minimal exposure to surrounding tissues. Radiosurgery at Virginia Mason Franciscan Health involves collaboration among a team of medical experts from neurosurgery, radiation oncology and diagnostic radiology.
- External beam radiation: This form of radiation therapy delivers radiation specifically to the area of the brain where the tumor is located, or it can be applied to the whole brain. A course of therapy often lasts five to six weeks.
-
Chemotherapy traditionally refers to drugs that damage the ability of cells to divide, usually by damaging their DNA. They can be taken orally or intravenously, and therefore they treat all the tumor cells in the body, but also impact organs like the bone marrow, GI tract, liver, hair, and other parts of the body where cells divide rapidly. Thankfully, more modern treatments have tended towards oral chemotherapies with fewer side effects.
Targeted therapy refers to drugs that are designed to specifically block a target signal in the cell. Cells have numerous and highly complex signaling pathways, and tumors will frequently have abnormal cellular signaling that can be targeted. Usually this is in the setting of a specific mutation that renders the cancer vulnerable to a particular targeted therapy. These therapies are more specific than traditional chemotherapy, but can also have side effects.
Immunotherapy refers to drugs that are designed to “unblock” the immune system from attacking the tumor. A natural function of the immune system, in addition to looking for foreign viruses, bacteria, or fungi in the body, is to look for abnormal cells or cancers and destroy them. Many cancers have developed specific systems for blocking the immune system from carrying out this function. Immunotherapy targets these blocking systems and unblocks the immune system, allowing it to destroy the cancer. Immunotherapy can have unwanted side effects by allowing the immune system to target normal tissue.
-
Tumor treating fields are a device worn on the head that consists of four pads placed on the scalp. The pads have leads that emit a low voltage alternating electrical current, that is not felt other than a mild sensation of heat on the scalp. They do not cause seizures or harm to the brain. The device works by making it difficult for tumor cells to divide properly. This has been shown in tumor cells in a lab dish and also has been studied in multiple phase 3 clinical trials in both newly diagnosed and recurrent glioblastoma. Tumor treating fields are currently under study for other brain tumors including metastases.
-
Treatment of your cancer or tumor will include more than just treating physical symptoms. Learn more about our comprehensive wellness and support services.
Find out more about new developments from the National Brain Tumor Society.